Medical Devices
Understanding Peripheral Arterial Disease Treatment with Below the Knee (BTK) Scaffolds
In the world of medical innovations, groundbreaking technology is quietly transforming the treatment landscape for Peripheral Arterial Disease (PAD). Known as Below the Knee (BTK) scaffolds, this treatment is designed to restore the ebb and flow of life to limbs which had once succumbed to pain and limitation. In this article, we explore the fascinating world of Below the Knee (BTK) scaffolds, a medical breakthrough to rewrite the fate of millions afflicted by PAD.
What is Peripheral Arterial Disease (PAD)?
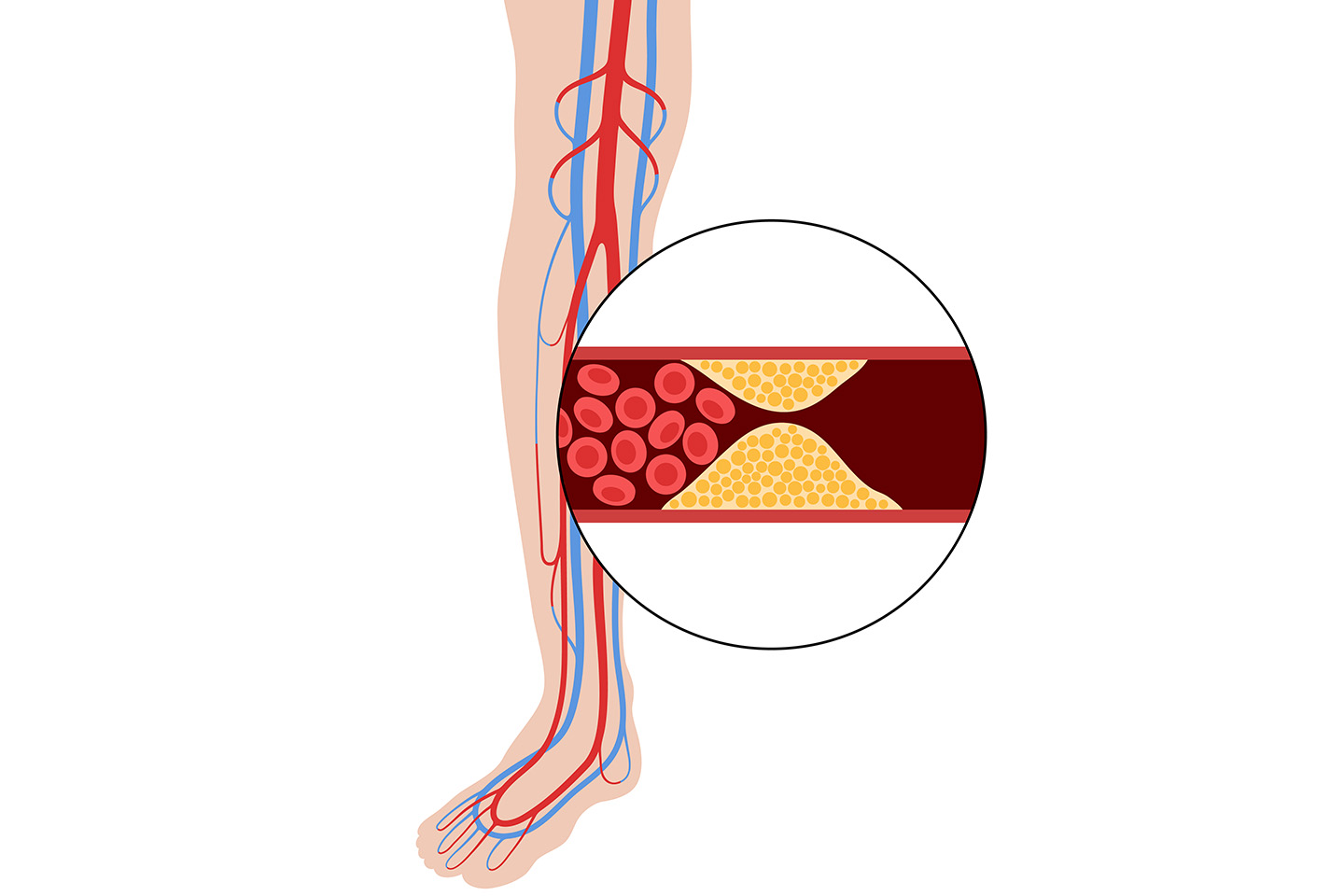
This debilitating condition occurs when plaque buildup in the arteries, restricting blood flow to the extremities, particularly the legs. If left untreated, PAD can lead to severe pain, ulcers, gangrene, and even amputations. While there have been significant advancements in the treatment of PAD, the development of Below the Knee (BTK) scaffolds is revolutionising the way we manage this condition. BTK scaffolds offer new hope for patients by providing targeted and innovative solutions to improve treatment outcomes.
What are BTK Scaffolds?
BTK scaffolds, also known as stents or endoprostheses, are medical devices used to prop open blocked or narrowed arteries in the lower extremities, especially below the knee. These scaffolds play a crucial role in restoring blood flow and preventing limb amputations in patients suffering from severe PAD. Unlike stents used in coronary arteries, BTK scaffolds are designed to address the unique challenges posed by the smaller and more intricate arteries found in the lower leg.
Types of BTK Scaffolds and Their Characteristics
Several types of BTK scaffolds are available, each with distinct characteristics catering to specific patient needs. The two main categories are bare-metal stents (BMS) and drug-eluting stents (DES). BMS are made of metal and provide structural support to keep the artery open. On the other hand, DES are coated with medications that are slowly released over time, reducing the risk of restenosis (re-narrowing of the artery). Both the types of BTK scaffolds have their advantages, and the choice depends on the individual patient's condition and medical history.
Mechanism of Action and Benefits of BTK Scaffolds in PAD Treatment
The mechanism of action of BTK scaffolds involves a minimally invasive procedure known as an endovascular intervention. During this procedure, the BTK scaffold is placed in the narrowed artery with the help of a catheter, which is threaded through a small incision. Once deployed, the scaffold expands, pushing the plaque against the artery walls, and remains in place, acting as a support structure to maintain blood flow.
The benefits of BTK scaffolds in PAD treatment are numerous:
- They provide a less invasive alternative to traditional open surgeries, reducing patient discomfort and recovery time significantly.
- They provide targeted treatment, precisely addressing the affected area and minimising damage to healthy tissues.
- BTK scaffolds have shown promising long-term results in preventing the recurrence of arterial blockages, preserving limb functionality, and finally improving the overall quality of life for patients.
Advancements in BTK Scaffold Technology
Breakthrough Materials and Design Innovations: Advancements in material science have led to the development of novel BTK scaffold materials that offer improved biocompatibility and reduced risk of adverse reactions. Innovations in scaffold design have also resulted in better flexibility, allowing for easier navigation through tortuous arteries, and enhanced radial strength to ensure the scaffold remains securely in place.
Bioresorbable and Drug-Eluting BTK Scaffolds: Bioresorbable BTK scaffolds represent a groundbreaking development in the field. These scaffolds are designed to be gradually absorbed by the body over time, leaving no permanent metallic implant behind. This feature addresses some of the limitations of traditional BMS, reducing the risk of long-term complications and facilitating potential future interventions. Additionally, drug-eluting BTK scaffolds, as mentioned earlier, have revolutionised treatment outcomes by reducing restenosis rates significantly and improving the long-term patency of the treated arteries.
Role of Nanotechnology in Improving Scaffold Performance: Nanotechnology has made notable contributions to enhancing the performance of BTK scaffolds. Incorporating nanoparticles into the scaffold's coating makes drug delivery more precise and targeted. Moreover, nanomaterials offer improved mechanical properties and better biocompatibility, further optimising the scaffold's overall effectiveness.
Efficacy
Comparative Analysis with Traditional Treatment Methods: When compared to traditional treatment methods like bypass surgeries or balloon angioplasty, BTK scaffolds have shown remarkable advantages. They have a lower risk of complications, shorter hospital stays, and faster recovery times. Moreover, their minimally invasive nature makes them a viable option for patients who are not suitable candidates for open surgeries.
Long-Term Outcomes and Patient Benefits: Studies evaluating the long-term outcomes of BTK scaffold treatments have reported encouraging results. Patients who have undergone BTK scaffold procedures experienced improved blood flow, reduced pain, and fewer ulcerations and gangrene. Furthermore, the preservation of limbs and the potential avoidance of amputations have significantly enhanced patients' overall quality of life.
Wrapping It Up
The advent of Below the Knee (BTK) scaffolds marks a crucial step forward in the treatment of Peripheral Arterial Disease (PAD). These innovative medical devices offer targeted and effective solutions which address the unique challenges posed by PAD in the lower extremities. As research and innovation progress, we can expect BTK scaffolds to play an increasingly pivotal role in transforming the lives of PAD patients and alleviating the burden of this debilitating condition globally.
FAQs
Q: How do BTK scaffolds work, and what benefits do they offer in PAD treatment?
A: BTK scaffolds work through a minimally invasive procedure called endovascular intervention. During this procedure, the scaffold is placed in the narrowed artery using a catheter, which is threaded through a small incision. The scaffold expands, pushing the plaque against the artery walls, and remains in place, providing structural support to maintain blood flow. The benefits of BTK scaffolds include less invasive treatment, targeted and precise intervention, and promising long-term outcomes in preventing artery blockages and improving overall limb functionality.
Q: What advancements have been made in BTK scaffold technology to enhance their performance?
A: Advancements in BTK scaffold technology include breakthrough materials and design innovations that improve biocompatibility, flexibility, and radial strength. Additionally, bioresorbable BTK scaffolds, which are gradually absorbed by the body over time, and drug-eluting BTK scaffolds, coated with medications to reduce restenosis, have contributed to better treatment outcomes. Furthermore, nanotechnology has significantly improved scaffold performance by enhancing drug delivery and mechanical properties.
Q: How do BTK scaffolds compare with traditional treatment methods, such as bypass surgeries or balloon angioplasty?
A: When compared to traditional treatment methods, BTK scaffolds have shown advantages, including a lower risk of complications, shorter hospital stays, and faster recovery times. Their minimally invasive nature makes them a viable option for patients who may not be suitable candidates for open surgeries. Moreover, BTK scaffolds have demonstrated sustained improvement in blood flow, reduced pain, and fewer instances of ulcerations and gangrene, leading to an enhanced overall quality of life for patients.
Q: Are BTK scaffold treatments suitable for all PAD patients, and what should patients consider before opting for this procedure?
A: BTK scaffold treatments may not be suitable for all PAD patients, as individual conditions can vary. Consulting qualified medical professionals is essential to determine each patient's most appropriate treatment approach. Factors such as the severity and location of arterial blockages, medical history, and overall health should be considered when evaluating the suitability of BTK scaffolds. Patients should have an informed discussion with their healthcare providers to understand the potential benefits and risks associated with this procedure and make an informed decision based on their unique circumstances.
References:
https://evtoday.com/articles/2019-may/peripheral-artery-disease-below-the-knee-unique-challenges-and-algorithmic-solutions
https://my.clevelandclinic.org/health/diseases/17357-peripheral-artery-disease-pad