Bicuspid Aortic Valve Disease – All You Need To Know
Introduction
Health disorders, especially those related to the heart, can cause long-lasting complications for the patient. These may be congenital or can develop throughout life. Irrespective of when one contracts a cardiovascular disorder, it should be attended to it immediately. A later diagnosis can result in complicated surgeries that may have life-long effects on the patient's health. One such cardiovascular disorder is the Bicuspid Aortic Valve Disease or BAVD. Let's understand what it is, its symptoms and treatment.
What is Bicuspid Aortic Valve Disease?
Bicuspid aortic valve disease is essentially a kind of irregularity in the aortic valve in the heart. It is generally a congenital condition.
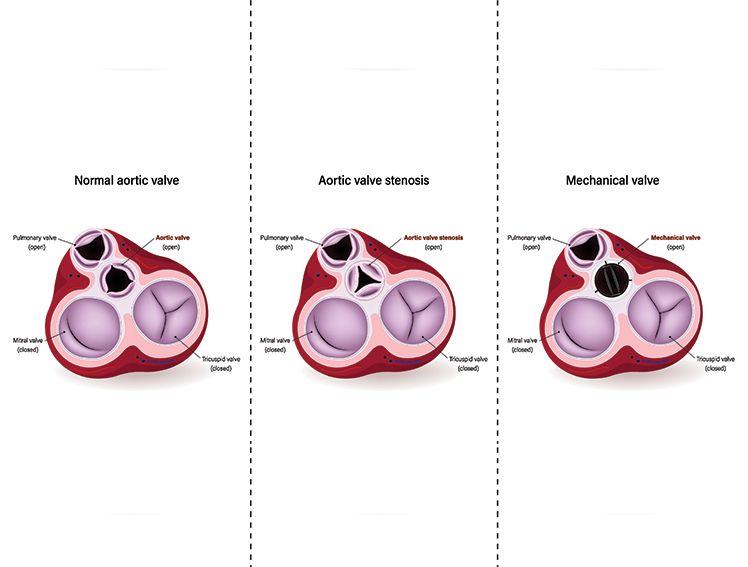
Your heart has four chambers. The two bottom chambers are called ventricles. The left ventricle is like a pump that pushes oxygen-rich blood through your main artery (called the aorta) to your entire body. Between this pumping chamber and your main artery, there's a door-like structure called the aortic valve that opens and closes to control blood flow. The four valves assist with the flow of blood through the four chambers of the heart and into the lungs or out to the body.
A normal aortic valve has three flaps (called leaflets) that work like a three-way door. In bicuspid aortic valve disease, you're born with only two flaps instead of three. This happens because the third flap doesn't form properly before birth, or two flaps grow together as one piece. The bicuspid valve opens and closes abnormally and may sometimes result in the valve leaking. The leakage allows the blood to flow back into the heart instead of the normal function of flowing forward into the body. This process, known as aortic regurgitation, makes the heart work harder.
Causes of Bicuspid Aortic Valve
Bicuspid aortic valve disease is primarily a genetic condition that can be inherited from one or both parents. Here's what causes it:
Genetic Factors: The condition tends to run in families. If one of your parents has a bicuspid aortic valve, you have a higher chance of having it too. Scientists have discovered that specific genes regulate the formation of heart valves during pregnancy.
Development During Pregnancy: The condition occurs when the baby's heart is forming in the womb, usually between the 6th and 9th week of pregnancy. During this critical time, the development of the valve leaflets may be affected.
Family History: About 7% to 9% of close family members (parents, children, siblings) of someone with a bicuspid aortic valve may also have the condition
Bicuspid Aortic Valve – Symptoms and Diagnosis
Even though you're born with bicuspid aortic valve disease, you might not notice any symptoms until you're an adult. As you get older, the valve can become narrowed (aortic stenosis) or may not close properly, leading to blood leaking backward (aortic regurgitation). When this happens, you might experience:
Early Symptoms:
Feeling tired more easily than usual
Getting out of breath during normal activities
Feeling dizzy or lightheaded
Chest discomfort or pain
Advanced Symptoms:
Severe shortness of breath, even when resting
Chest pain that gets worse with activity
Fainting or near-fainting episodes
Rapid or irregular heartbeat
Swelling in your feet, ankles, or legs
When to See a Doctor Immediately: If you experience severe chest pain, difficulty breathing, or fainting, seek emergency medical care right away.
When you visit your doctor with symptoms, they will use several tests to diagnose bicuspid aortic valve disease:
Physical Examination: Your doctor will listen to your heart with a stethoscope. A bicuspid aortic valve often creates a heart murmur (an extra sound) that trained doctors can hear.
Echocardiogram (Echo): This is like an ultrasound for your heart. A technician places a device on your chest that uses sound waves to create moving pictures of your heart. This test shows how well your valve opens and closes and if blood is leaking backward.
Transesophageal Echocardiogram (TEE): If doctors need clearer pictures, they might do this special ultrasound. You'll swallow a thin, flexible tube with an ultrasound device that takes pictures from inside your throat. This gives very detailed images of your valve.
Electrocardiogram (EKG or ECG): This test records your heart's electrical activity using sticky pads placed on your chest. It shows if your heart rhythm is normal and if your heart muscle is working harder than usual.
Chest X-ray: A simple X-ray picture of your chest shows the size and shape of your heart and checks your lungs for any problems.
Advanced Imaging:
- Cardiac CT Scan: Takes detailed 3D pictures of your heart and blood vessels
- Cardiac MRI: Uses magnetic fields to create very detailed images of your heart structure and function
Bicuspid Aortic Valve Treatment
Treatment depends on how well your valve is working and whether you have symptoms. Your doctor will create a personalised treatment plan based on your specific situation.
Monitoring and Medication: If your valve is working fairly well and you don't have symptoms, your doctor may recommend:
- Regular check-ups with echocardiograms to monitor the valve
- Medications to help your heart work more efficiently
- Lifestyle changes like regular exercise and a heart-healthy diet
Minimally Invasive Procedures:
If the valve function worsens, the patient may need to undergo a procedure, which could be:
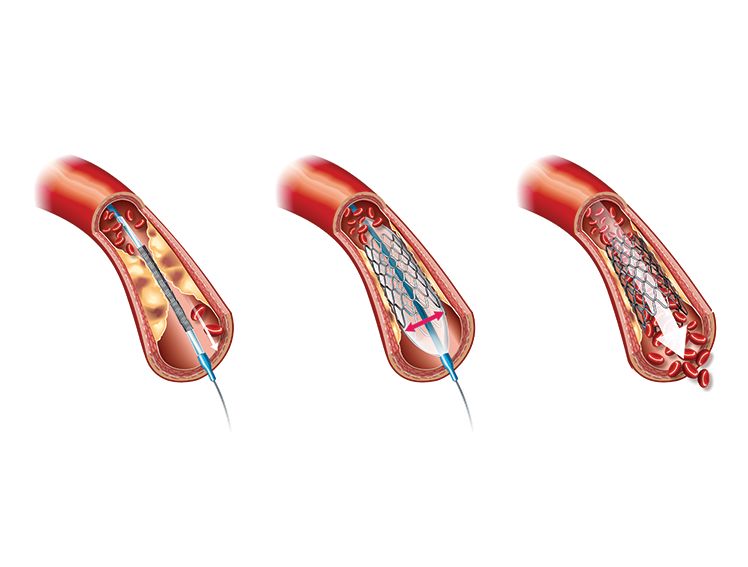
Balloon Valvuloplasty: This is like opening a blocked drain. Your doctor inserts a thin, flexible tube (catheter) through a blood vessel in your leg and guides it to your heart. A small balloon at the tip is inflated inside the narrow valve opening to stretch it wider, then removed. This procedure can improve blood flow temporarily but may need to be repeated.
TAVR (Transcatheter Aortic Valve Replacement): This newer procedure replaces your valve without open-heart surgery. A new valve is inserted through a catheter and positioned inside your existing valve. Recovery time is typically shorter than traditional surgery.
Surgical Options:
Valve Repair: Surgeons can fix your existing valve by reshaping or tightening the leaflets with special stitches. This preserves your natural valve when possible.
Valve Replacement: When repair isn't possible, your surgeon will replace the valve with either:
- Mechanical Valve: A durable artificial valve that is durable and long lasting but requires blood-thinning medication
- Tissue Valve: Made from animal tissue, do not require long-term blood thinners but may eventually need replacement
Ross Procedure: Your surgeon moves your pulmonary valve (from the right side of your heart) to replace your aortic valve, then puts an artificial valve where your pulmonary valve used to be.
Living with Bicuspid Aortic Valve Disease:
Having bicuspid aortic valve disease doesn't mean you can't live a full, active life. Here's what you need to know:
Regular Follow-up Care:
See your cardiologist regularly, even if you feel fine
Get echocardiograms as recommended
Take all medications as prescribed
Lifestyle Recommendations:
Exercise: Most people can exercise normally, but check with your doctor first
Diet: Follow a heart-healthy diet low in salt and saturated fat
Dental Care: Tell your dentist about your valve condition before any dental procedures
Family Screening: Since a bicuspid aortic valve can run in families, your close relatives should consider screening with an echocardiogram.
Pregnancy Considerations: Women with a bicuspid aortic valve can usually have safe pregnancies with proper medical monitoring.
Final Note
Bicuspid aortic valve disease is manageable when caught early and treated properly. If you have a family history of this condition, get screened with an echocardiogram. Don't ignore symptoms like chest pain or shortness of breath, and keep regular appointments with your heart doctor. Many people with a bicuspid aortic valve live full, active lives with proper medical care. Consult your doctor if you experience chronic chest or back pain, racing heartbeats, shortness of breath, or unexplained and persistent fevers.