Do All PCI Procedures Involve Stents? Here's What You Need to Know
Introduction
When it comes to heart treatments, especially for blocked arteries, one common term you might hear is percutaneous coronary intervention. A lot of people ask, "Does every PCI involve a stent?" The short answer is no. Let's explore what PCI is, how it works, and when stents are used.
What Is Percutaneous coronary intervention (PCI)?
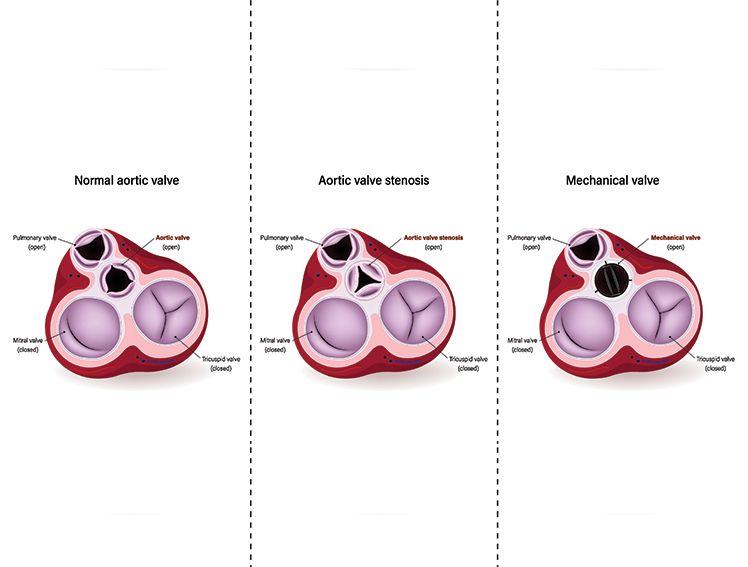
Percutaneous coronary intervention, or PCI, is a medical procedure that helps open up blocked or narrowed blood vessels in the heart. These blood vessels, called coronary arteries, carry oxygen-rich blood to your heart muscles. When these arteries become narrow or blocked due to fatty deposits (also known as plaque), it can cause chest pain or even a heart attack. PCI helps treat this problem without needing open-heart surgery. Doctors use a thin tube called a catheter to reach the heart through a blood vessel, usually from the wrist or groin.
Understanding the Role of PCI in Heart Treatment
The goal of percutaneous coronary intervention is to restore blood flow to the heart. When blood can't flow freely due to blockages, the heart doesn't get enough oxygen.[1] This can lead to serious symptoms like chest pain, shortness of breath, or a heart attack. PCI helps alleviate this by opening the blockage, which relieves symptoms and improves heart function. It's a quicker and less invasive option compared to surgery, which means recovery is also usually faster.
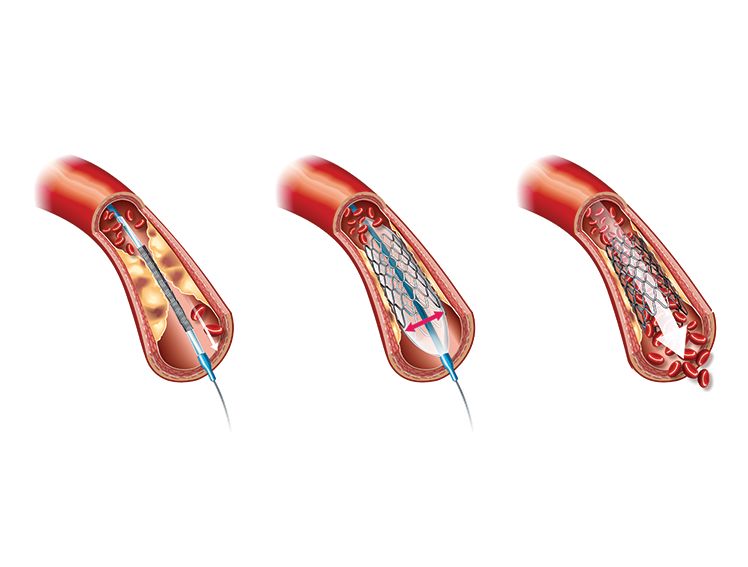
What Is a Stent and How Does It Work?
A stent is a tiny mesh-like metal tube. After the blocked artery is opened using a balloon during PCI, a stent is sometimes placed in that area to keep the artery open. Think of it like placing a small support inside the pipe to keep it from closing again. Some stents are even coated with medicine that helps prevent the artery from narrowing again. Once placed, the stent stays inside the artery permanently and becomes part of the artery wall over time.
Does Every PCI Use a Stent? The Short Answer: No
No, not all percutaneous coronary intervention procedures involve placing a stent. While stents are commonly used, they are not always necessary. In some cases, the artery can be opened successfully using just a balloon, and the doctor may decide not to place a stent. This depends on the condition of the artery and how well it stays open after the balloon is removed.
When Is a Stent Typically Used?
Stents are used in 80-90% of PCIs[2] for severe stenosis (>70%), unstable angina/ACS, or high-restenosis risk (e.g., diabetes). or if there is a risk that the artery might close again. If balloon angioplasty alone doesn't give good results, a stent is placed to support the artery[3]. Stents are also commonly used after a heart attack, where quick restoration of blood flow is important. In many cases, using a stent helps prevent future blockages and gives better long-term outcomes.
Benefits and Limitations of Using Stents
There are several benefits of using stents. They help keep the artery open, improve blood flow, and reduce symptoms like chest pain. Patients often recover faster compared to those who undergo surgery. However, there are also some limitations. Sometimes the artery can become narrow again, or blood clots can form near the stent. That's why people with stents are often asked to take certain medicines to reduce the risk of clotting. So, while stents are helpful, they are not always the perfect solution for everyone.
How Doctors Decide on Stents
Doctors carefully consider many factors before deciding whether to use a stent during percutaneous coronary intervention. They assess the size, location, and severity of the blockage, as well as how well the artery remains open after using a balloon. If the artery looks stable without a stent, they might avoid using one. Doctors also use specialised imaging tools during the procedure to gain a clearer view inside the artery and determine the best approach. Every patient is different, so the decision is made based on individual health conditions and the expected benefits.
What Patients Should Know and Ask
If you or a loved one is going through percutaneous coronary intervention, it's important to understand what the procedure involves. Don't hesitate to ask your doctor questions like: Will a stent be used in my case? Are there any risks with or without a stent? What kind of medicines will I need afterwards? How can I take care of my heart after the procedure? Being involved in your treatment helps you feel more confident and informed, and it also helps you make better health choices in the future.
Meres100 by Meril Life
MeRes100™ by Meril Life is a next-generation PLLA-based bioresorbable scaffold that treats blocked arteries without staying in the body permanently. Unlike metal stents, it supports the artery, releases medicine to prevent re-blockage, and then naturally dissolves in about two to three years. Its thin design helps the artery heal better and reduces long-term risks.
BioMime by Meril Life
BioMime is a sirolimus-eluting DES with 65 µm struts and biodegradable polymer, used to open blocked arteries. It is very thin and flexible, allowing it to fit well inside the artery. It slowly releases medicine to keep the artery from getting blocked again. Over time, its coating naturally fades away, helping the artery heal more effectively.
Evermine by Meril Life
Evermine50 by Meril Life is an everolimus-eluting DES with 50 µm struts heart stent used to treat blocked arteries. It helps open the blood vessels and slowly releases the medicine to prevent the blockage from returning. Because it's so thin and flexible, it causes less damage and helps the artery heal faster. It's designed to be both strong and gentle, making it safer and more effective for patients with heart conditions.
Conclusion
So, does every PCI involve a stent? Not always. While stents are commonly used, not all percutaneous coronary intervention procedures require one. Sometimes, balloon angioplasty or other techniques are enough. The best treatment depends on your specific condition, and your doctor will choose what's safest and most effective for you. What matters most is understanding the options and staying informed, so you can take the best care of your heart.
References