Hemorrhoidectomy
What is hemorrhoidectomy?
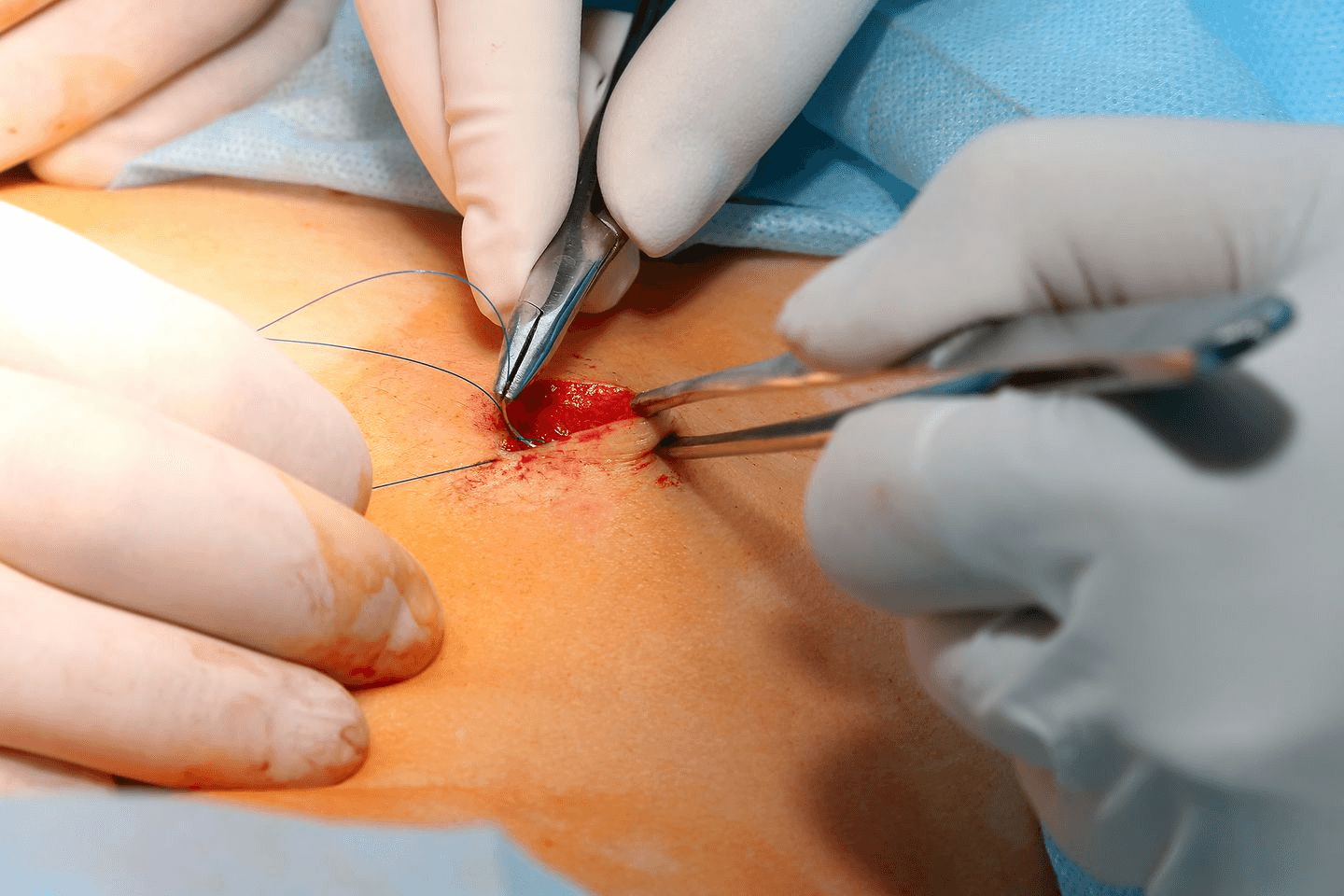
Hemorrhoidectomy is a surgical procedure that involves the complete removal of hemorrhoidal tissue through various cutting techniques. During the operation, surgeons excise the problematic hemorrhoidal bundles and seal the blood vessels to prevent bleeding.[1]
The procedure is performed under anesthesia and most hemorrhoidectomies are outpatient procedures, allowing patients to return home the same day.[1]
Most hemorrhoids respond well to conservative treatments including dietary changes, topical medications, and lifestyle modifications. However, hemorrhoidectomy surgery becomes necessary when these approaches fail to provide adequate relief or when complications develop.[6][8]
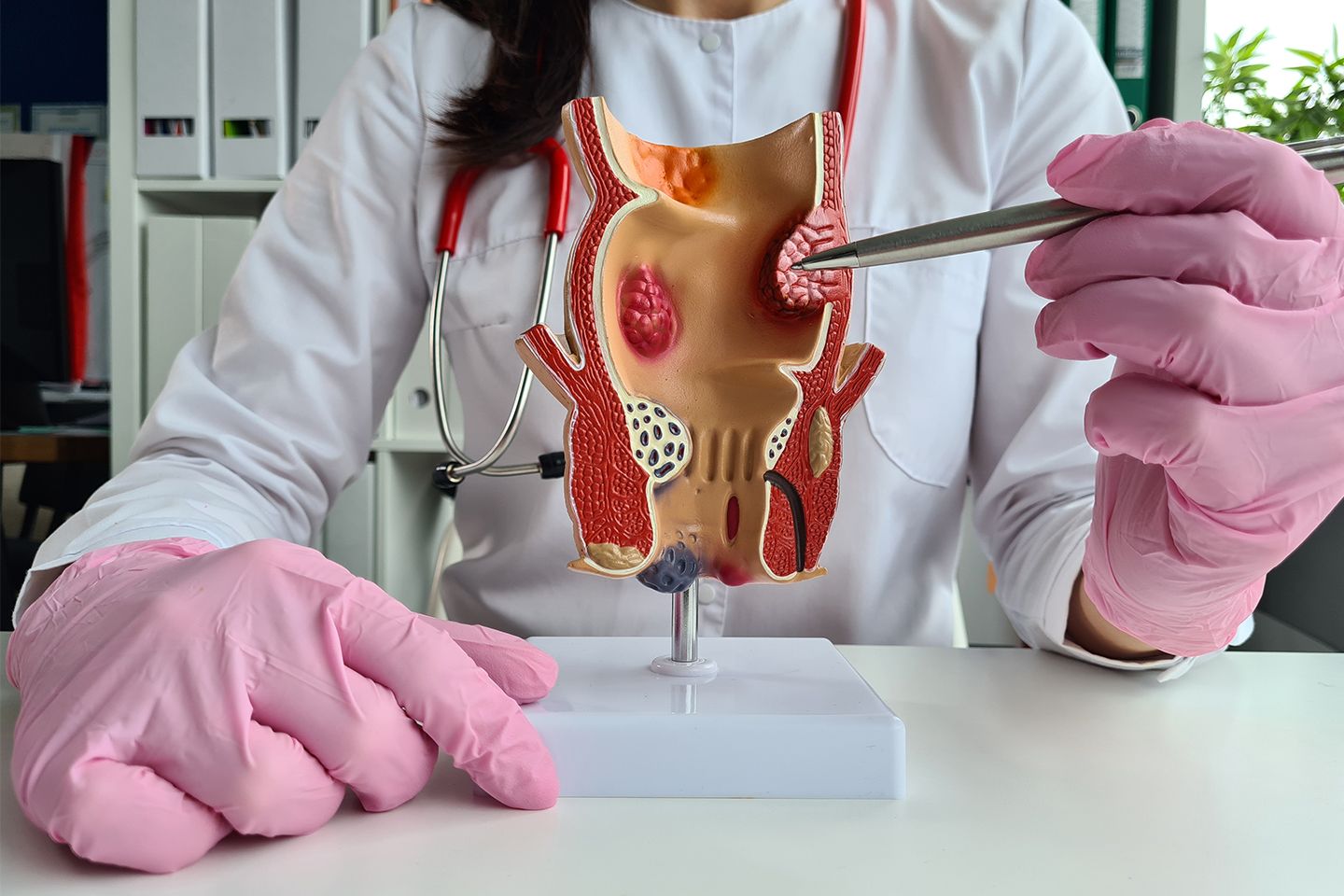
Types of Hemorrhoids
Internal: Internal hemorrhoids develop inside the anal canal and rectum, above the dentate line. These are typically painless because this area has fewer nerve endings, but they can cause bleeding during bowel movements.[8] Internal hemorrhoids are classified into four grades based on their severity:[3]
- Grade 1: Hemorrhoids that bleed but don't prolapse
- Grade 2: Prolapse during bowel movements but return spontaneously
- Grade 3: Prolapse and requires manual repositioning
- Grade 4: Permanently prolapsed and cannot be repositioned
External: External hemorrhoids form below the dentate line around the anal opening where nerve endings are more abundant, making them typically more painful than internal ones.[6][8] These hemorrhoids can cause intense discomfort, especially when thrombosed (blood clot formation occurs), leading to severe pain and swelling.[1] The patient may develop a clot in external hemorrhoids or thrombosis (formation of blood clots). They are not dangerous but can cause a lot of discomforts.
Prolapsed: When internal or external hemorrhoids protrude out of the rectum, they are called 'prolapsed.' The patient may experience lumps on the anus, itching, irritation, bleeding, inability to defecate properly (bowels do not feel empty), faecal leakage, and/or mucus discharge that emits an unpleasant odour.[8]
Who needs a hemorrhoidectomy?
Healthcare providers typically recommend hemorrhoidectomy surgery for patients with:
- Grade III or IV internal hemorrhoids that cause persistent symptoms
- Mixed internal and external hemorrhoids affecting quality of life
- Thrombosed external hemorrhoids causing severe pain
- Strangulated internal hemorrhoids with compromised blood supply
- Failed response to minimally invasive treatments like rubber band ligation
- Chronic bleeding leading to anemia
- Recurrent prolapse interfering with daily activities
The UCF Center for Colorectal Surgery states that people experiencing Grade 3, Grade 4, and a mix of internal and external hemorrhoids require a hemorrhoidectomy.[7] Those with strangulated internal hemorrhoids (blood clot forms here), thrombosed external hemorrhoids, and unable to tolerate general pain of the hemorrhoids or minimally invasive interventions need hemorrhoidectomy.[7]
Types of hemorrhoidectomy
There are different types of hemorrhoidectomy like:
- Closed Hemorrhoidectomy: Closed hemorrhoidectomy represents the most commonly performed hemorrhoidectomy procedure.[1] The surgeon makes precise incisions around the hemorrhoidal tissue using surgical instruments, removes the affected tissue, and closes the wounds with absorbable sutures. These sutures absorb into the skin over time.
- Open Hemorrhoidectomy: Open hemorrhoidectomy follows the same surgical approach but leaves the wounds open to heal naturally. This method may be chosen when wound closure is technically challenging due to location or when patients have certain medical conditions that affect healing.[4]
- Stapled Hemorrhoidectomy: Stapled hemorrhoidopexy, also known as Procedure for Prolapse and Hemorrhoids (PPH), uses a circular stapling device to reposition hemorrhoidal tissue rather than removing it completely.[4][6] The stapler cuts away excess tissue and lifts the remaining hemorrhoids back into their normal anatomical position within the anal canal.[4] This technique typically results in less post-operative pain and faster recovery compared to traditional excisional methods. This step is usually taken for patients who have grade III and IV hemorrhoids or for whom minimally invasive techniques have not yielded the expected results.[4][5]
How long does it take to recover from a hemorrhoidectomy?
The patient is usually given general anesthesia, so they are unconscious during the procedure, and the muscles are relaxed so they cannot feel the pain.[1] However, the pain is experienced after the patient wakes up. Usually, patients can go back home on the same day with their caregiver unless the doctor does not see them as fit to leave.[5] Patients are also asked to take stool softeners for a brief while so they can poop easily.[6] Besides this, they are also advised to eat fiber-rich food and take fiber supplements to avoid constipation.[8] Sitting in a sitz bath, using a cold compress, and taking painkillers are also part of the post-surgery plan.[2][5] Patients may or may not experience some after-effects of the anesthesia. The recovery period differs from person to person, but the usual time is about a week or two.[1] Stitches of the surgery will dissolve into the skin on their own. The doctor will also schedule a follow-up to check on the progress post-surgery.[1][2]
MIRUS Hemorrhoids Stapler By Meril
MIRUSTMHEMORRHOIDS STAPLER: MIRUSTM HEMORRHOIDS STAPLER by Meril Life is used for the hemorrhoidectomy of internal and external hemorrhoids and thrombosed hemorrhoids. It is also used for Minimally Invasive Procedures for Hemorrhoids (MIPH) and Stapled Transanal Resection of Rectum (STARR). This device ensures security and clean hemostasis and is easy to use. It gives optimised staple formation with adjustable height staples.
Just like any surgery, a hemorrhoidectomy is also a major procedure. Going under the knife and being administered anesthesia can be daunting for the patient, but if they are well-versed with all aspects of the surgery and its after-effects, they can go with a calm state of mind. This surgical procedure has few risks and has been proven safe and effective in combating hemorrhoids.
Following your doctor's instructions after the surgery is essential, and maintaining a balanced diet with plenty of fruits and vegetables will only be beneficial in the long run. Also, ensure that you avoid sitting in one spot for an extended period, especially if you have a desk job. This will reduce any chances of hemorrhoids or their
References
[1] https://medlineplus.gov/ency/article/002939.htm
[2] https://www.medindia.net/health/surgical-procedure/hemorrhoidectomy.htm
[3] https://surgery.ucsf.edu/procedure/hemorrhoidectomy
[4] https://www.medicalnewstoday.com/articles/324439
[5] https://resources.healthgrades.com/right-care/hemorrhoid-surgery
[6] https://www.webmd.com/digestive-disorders/surgery-treat-hemorrhoids
[8] https://www.health.harvard.edu/diseases-and-conditions/hemorrhoids_and_what_to_do_about_them