Diabetes-Related Foot Problems: What You Need to Know
Introduction
Diabetes can, when not managed, affect parts of your body, but your feet face the most significant risk. If you have high blood sugar, it can lead to nerve damage, poor blood flow, and a range of foot problems that many people overlook at first. These may start small, a tiny cut, blister or patch of dry skin, but can turn serious if ignored.
This article explains why diabetes affects the feet, the common problems people experience, the warning signs to watch for, and how doctors diagnose and manage these conditions. We'll also share practical tips to protect your feet every day.
Why Diabetes Affects the Feet
Feet are particularly vulnerable because diabetes can cause:
1. Nerve Damage (Diabetic Neuropathy)
High blood sugar, if chronic, can damage nerves, especially in the legs and feet. It reduces your ability to feel pain, heat or injury. Someone may not notice a stone in their shoe or a small cut until it becomes infected.[1]
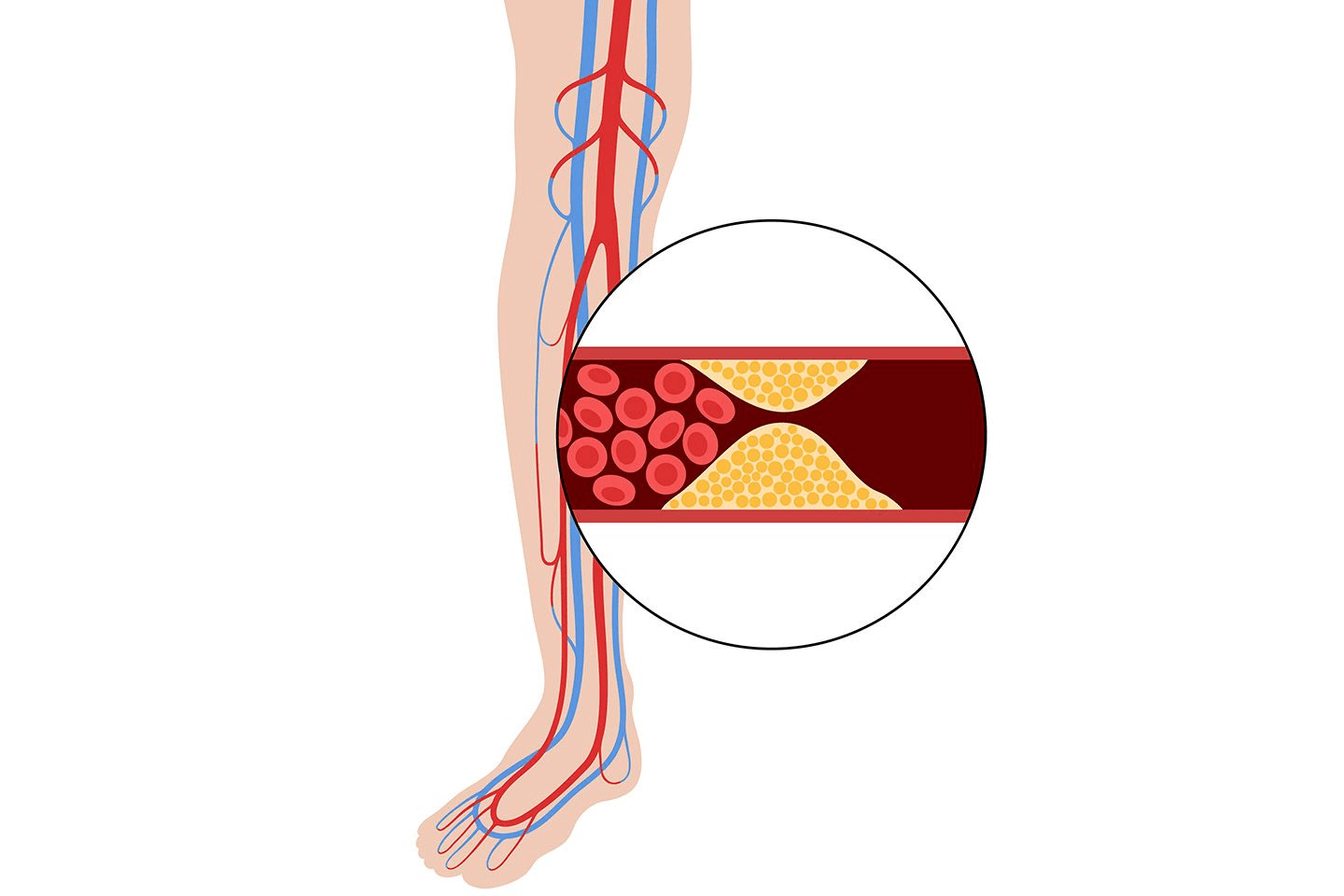
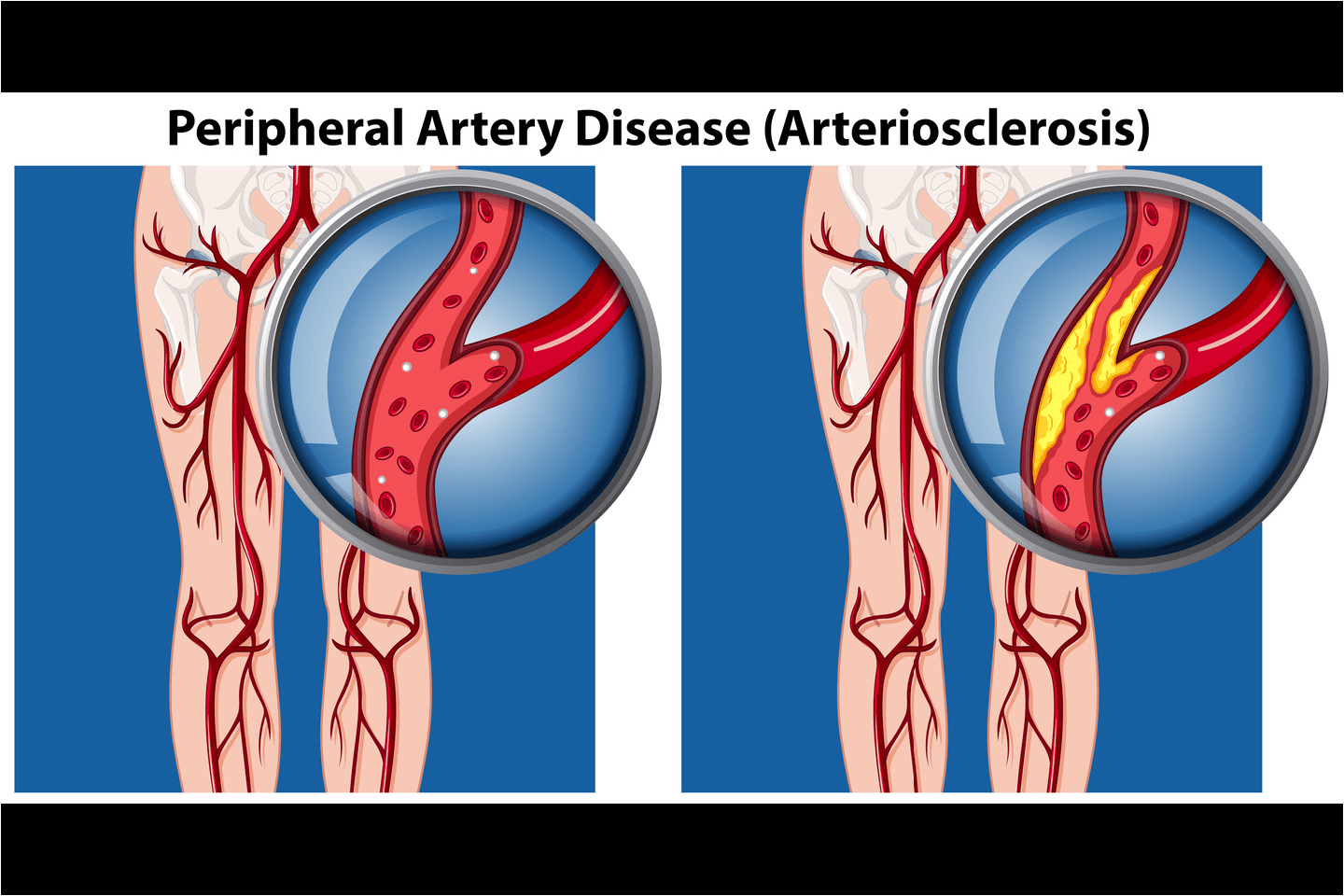
2. Poor Circulation
Diabetes may affect your blood vessels, reducing blood flow to your feet. When circulation is poor, wounds heal slowly, infections spread faster, and tissues are more likely to break down. Both neuropathy and reduced circulation create the perfect conditions for serious foot complications.
Common Foot Problems Caused by Diabetes
People with diabetes may experience different foot issues, some minor, some serious, but all require attention.
Nerve Damage and Loss of Sensation
Neuropathy may cause tingling, burning, numbness or complete loss of sensation. Without pain to alert you, injuries often go unnoticed.
Sores and Blisters
Ill-fitting shoes or friction may lead to blisters and sores. When you cannot feel discomfort, these can worsen quietly.
Infections in Wounds
Cuts, cracks, or blisters can easily become infected, especially when bacteria enter through broken skin. Because blood flow is reduced, your body struggles to fight infections.
Slow Healing Wounds
Poor circulation means wounds take longer to heal. If untreated, tissues can die due to a lack of oxygen and nutrients, a condition called gangrene.
Foot Ulcers
Around 15% of people with diabetes develop foot or toe ulcers at some point.[2] These open sores can form under calluses, on pressure points, or after small injuries. If left untreated, ulcers may deepen and become infected.
Other Common Problems
Diabetes also increases the risk of:
Corns and calluses
Fungal infections
Ingrown toenails
Bunions
Cracked heels
Burns from hot water or heating pads due to reduced sensation
These may seem small, but in a diabetic foot, even minor issues can become major complications.
Warning Signs to Watch Out For
Early detection can prevent serious consequences. Look out for:
Swelling in the feet or ankles
Foot pain or discomfort
Discolouration (red, blue, purple or pale skin)
Numbness or tingling
Warmth in one area
Open wounds that do not heal
Deformed foot shape (in advanced neuropathy)
Signs of Charcot foot – a rare but serious condition where weakened bones and joints collapse
Blackened skin, which may indicate gangrene and requires urgent medical care
Diagnosis: What Your Doctor May Do
If you report any symptoms, your doctor will examine your feet, check sensation using a simple monofilament test, and assess blood flow. If needed, they may advise X-rays to look for bone or joint damage.
Treatment and Management
Treatment depends on the condition diagnosed, but early care is vital.
Cleaning and Treating Wounds
Doctors may:
Clean the wound gently
Drain any pus
Remove dead or infected tissue (a process called debridement)
Apply dressings designed to absorb extra fluid and protect healing skin
Managing Infections
If infections are present, you may need topical, oral or even IV antibiotics depending on severity.
Reducing Pressure on the Foot
Doctors might recommend special footwear, crutches or wheelchairs to reduce pressure to help wounds heal faster (called offloading).
Diabetes Testing and Why It Matters
Monitoring your glucose levels helps prevent future complications. Common tests include:
Fasting blood glucose tests – measure sugar levels after overnight fasting
Oral Glucose Tolerance Test (OGTT) – checks how your body handles sugar
HbA1c testing – tracks your average glucose over the past 2–3 months.
For accurate and reliable HbA1c measurement, GluQuant A1c can support healthcare professionals in assessing long-term control.
Preventive Foot Care Tips
Prevention is always better than a cure. Here are simple daily habits:
Check your feet every day for cuts, blisters, redness or swelling
Wash and dry thoroughly, especially between toes
Moisturise dry skin, but avoid between the toes
Trim nails straight across [3]
Wear comfortable, well-fitted shoes
Avoid walking barefoot
Keep blood sugar under control
Get regular foot exams from your healthcare provider
Small efforts today can prevent big complications tomorrow.
Conclusion
Diabetes-related foot problems are common but can be managed effectively with awareness, early diagnosis and proper care. By understanding why these issues occur, recognising warning signs and following preventive steps, you can protect your feet and maintain overall health. If you ever notice anything unusual, no matter how small, speak to your doctor promptly.