Malaria Diagnosis Guide: Test Types, Results & Patient Tips
Introduction
Malaria diagnosis is a critical first step when a patient presents with fever, chills, or unexplained illness in endemic regions. Timely testing helps guide further investigations, confirm infection, and support appropriate treatment decisions. This guide explains how malaria is diagnosed, what tests are used, and how results are interpreted for both patients and healthcare providers.
Common Malaria Test Options & Clinical Use of Rapid Tests
When malaria is suspected, diagnosis typically follows a stepwise approach: screening tests are performed in hospitals or diagnostic laboratories, followed by confirmatory investigations.
Malaria Rapid Test Kits
Malaria rapid test kits are widely used as initial screening tools in clinical settings. These tests:
Detect specific antigens (proteins) of the malaria parasite
Provide results within 15–30 minutes
Are useful in both urban hospitals and resource-limited healthcare facilities
May not detect very low parasite levels, making confirmatory testing essential
Rapid tests are intended for use under clinical supervision to ensure proper sample collection, interpretation, and follow-up.
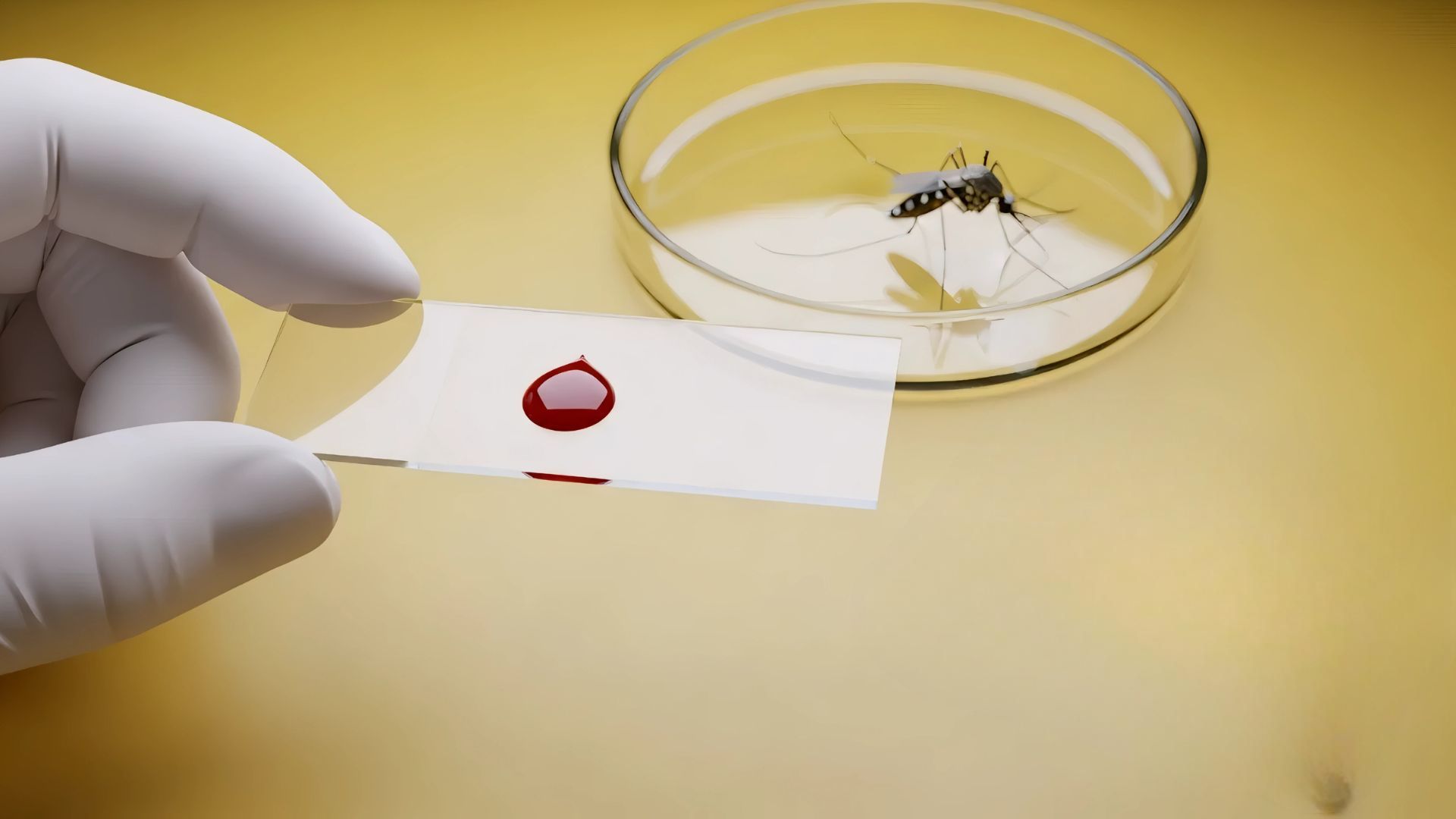
Confirmatory Laboratory Tests
To confirm malaria infection and guide further care, laboratory-based tests are used:
Complete Blood Count (CBC): Assesses anemia, platelet levels, and overall blood health, often altered in malaria
Microscopic blood smear (thick and thin films): Identifies malaria parasites, determines species (Plasmodium falciparum, P. vivax), and estimates parasite density
Malaria ELISA: Increasingly used, especially in blood banks, to screen donated blood and prevent transfusion-related malaria
Molecular tests (PCR): Highly sensitive tests that detect low-level or mixed infections in specialized laboratories
This screening-plus-confirmation pathway improves diagnostic accuracy, and supports timely and appropriate treatment.
Comparison of Major Malaria Test Methods
Test Method | Typical Time to Result | Primary Role | Key Use / Strength |
Malaria Rapid Diagnostic Test (RDT) | 15–30 minutes | Screening | Rapid detection of malaria antigens with minimal equipment |
Peripheral Blood Smear (Thick & Thin Film) | A few hours | Confirmatory (Reference Standard) | Confirms malaria, identifies species, estimates parasite density |
PCR (Molecular Testing) | Several hours | Reference / Confirmatory (Specialized use) | High-sensitivity detection, including low-level parasitemia |
Why Malaria Testing Matters Beyond Fever Diagnosis
Malaria testing does more than identify the cause of fever. It also helps:
Rule out other infections, such as dengue or typhoid
Decide whether further investigations are required
Support surveillance and prevalence monitoring
Reduce inappropriate or unnecessary antimalarial use
Early and accurate diagnosis improves patient outcomes and supports responsible healthcare practices.
Before You Undergo a Malaria Test
Share recent travel or exposure history
Mention when symptoms began and how they progressed
Avoid starting antimalarial medication unless advised by a doctor
Carry previous test reports if undergoing repeat evaluation
Testing should always be performed in recognized hospitals or diagnostic laboratories to ensure accurate results.
Understanding Malaria Test Results
If the test is positive:
Confirms the presence of malaria antigens or parasites
Species identification (via lab tests) helps guide next steps
If the test is negative:
Fever may have another cause
Repeat testing or additional investigations may be required if symptoms persist
Results should always be interpreted alongside clinical findings.
Tips for Interpreting & Acting on Results
Use both symptoms and test findings for decision-making
Repeat tests if results are inconclusive
Record species and parasite levels when available
Do not rely on suspicion alone for treatment decisions
Conclusion
Malaria diagnosis is most effective when rapid screening tests are supported by appropriate confirmatory laboratory investigations. While rapid tests help in early detection and timely decision-making, confirmatory methods such as blood smear examination and molecular testing provide clarity on infection status, species identification, and disease severity. Interpreting results alongside clinical symptoms and exposure history is essential to ensure accurate diagnosis, appropriate treatment, and safer patient care.