Peripheral Artery Disease (PAD): Symptoms You Shouldn’t Ignore and Impacts on Daily Life
Introduction
Peripheral artery disease (PAD) is commonly associated with leg pain, but it is more than just that.
PAD is a progressive vascular condition[1], the prevalence of which has increased globally[2], highlighting a significant public health concern in recent years.
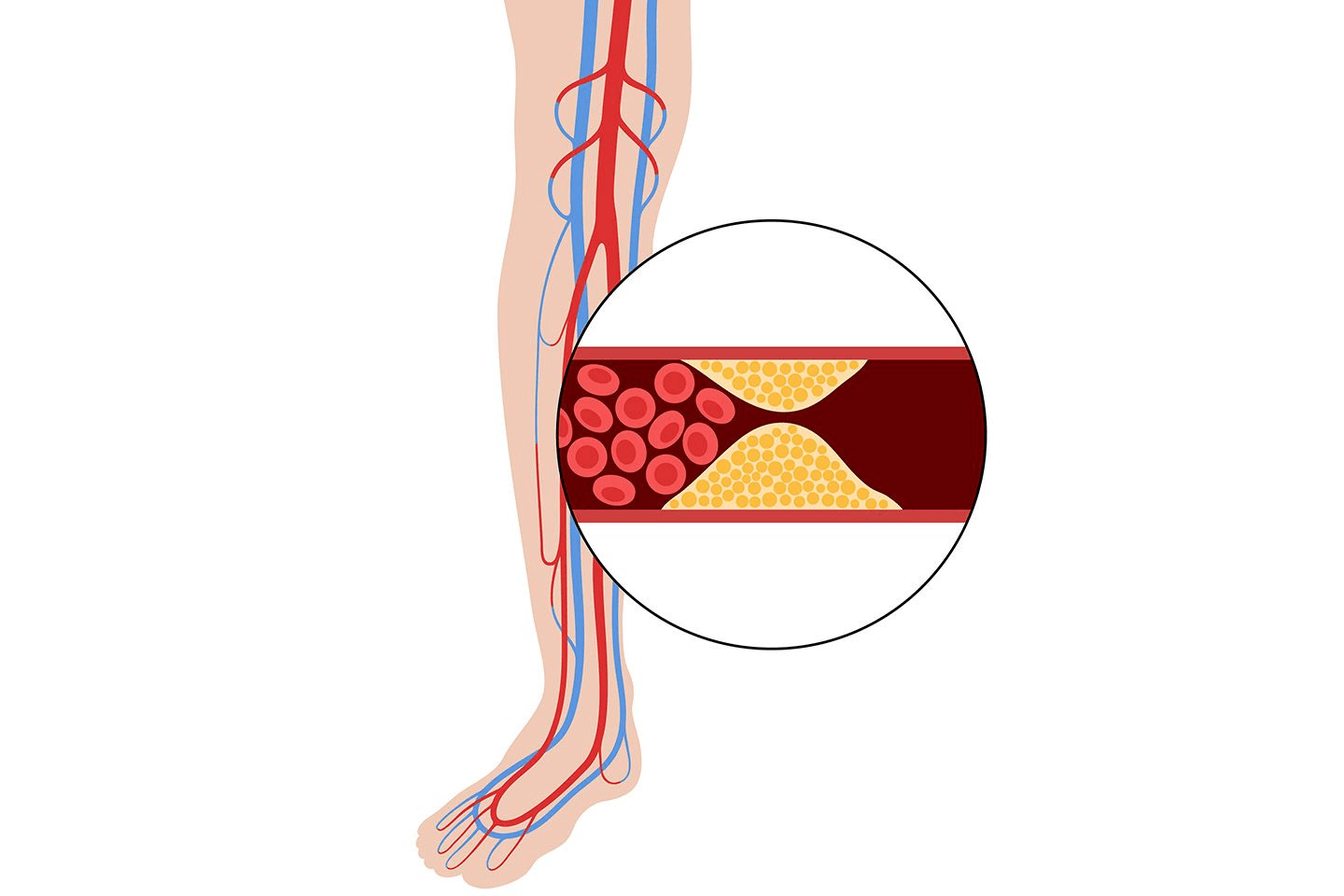
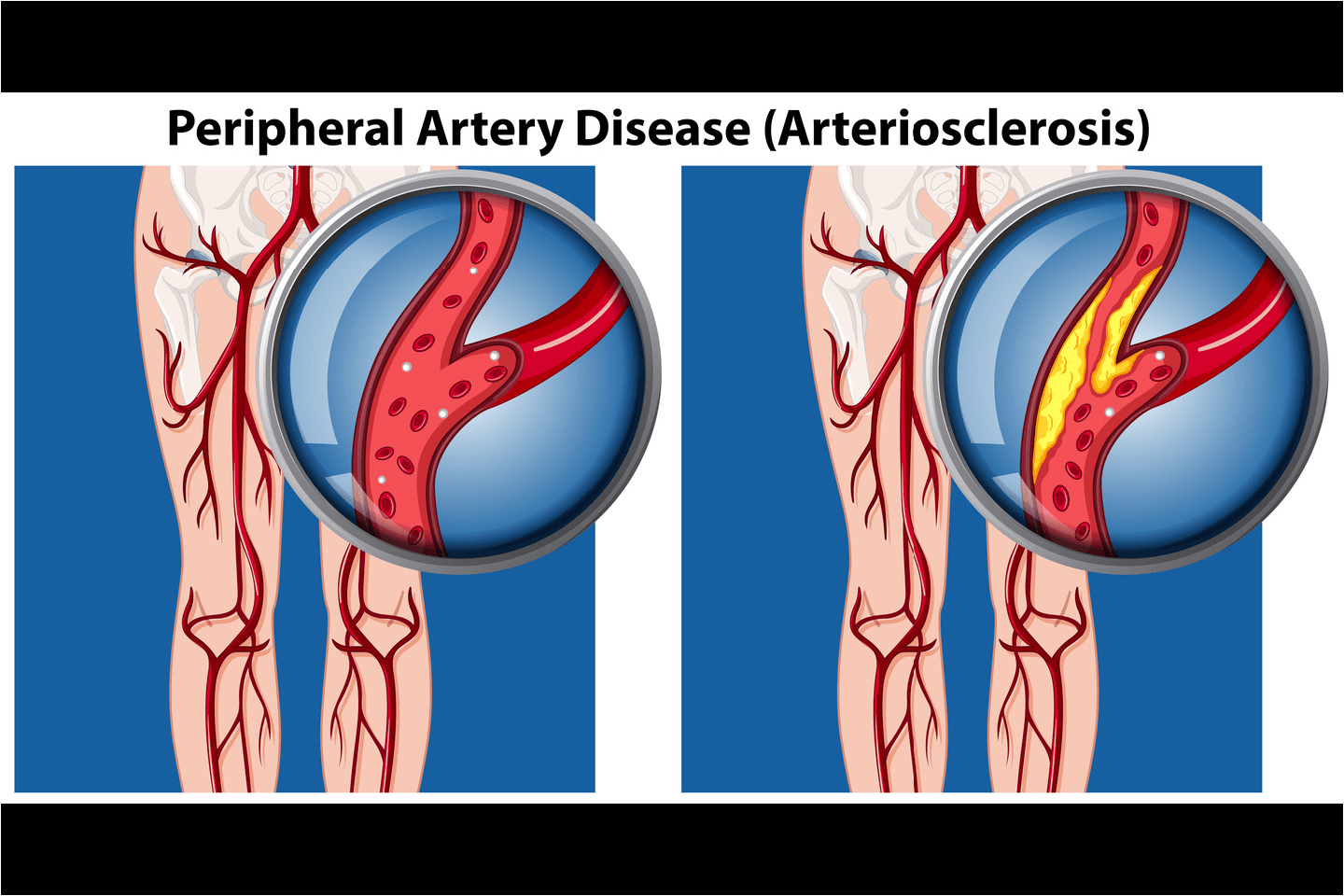
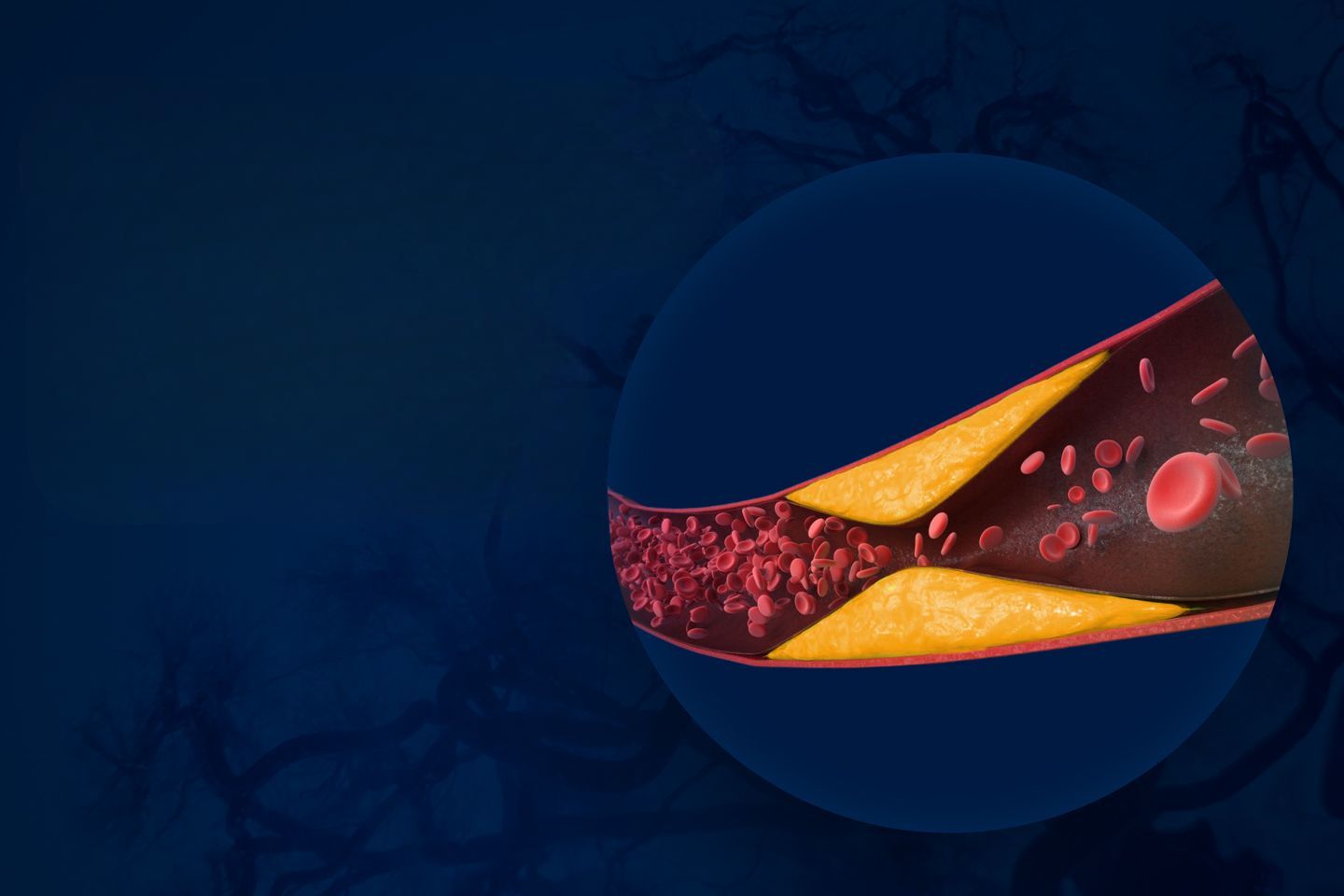
Peripheral Artery Disease is caused when a buildup of cholesterol and fats[1] in the arteries – a condition known as atherosclerosis – causes them to become narrow, restricting blood flow[1]. This buildup is commonly called plaque and the condition can dramatically reduce a person’s quality of life[3]. If overlooked, it can also lead to serious consequences.[3]
Symptoms to Watch Out For
PAD arises when arteries supplying blood to the limbs, most commonly the legs[1], become narrow due to atherosclerosis[2], cutting down oxygen delivery to muscles and tissues. Unfortunately, nearly 40% of people with PAD show no pain-related symptoms, and many others may have a confusing set of atypical symptoms[5]. Some patients may also dismiss[6] some of the early symptoms due to ignorance, until it is too late.
Detecting and managing PAD in time is critical, as patients are at the same level of cardiovascular risk[5] as those who have suffered previous cardiac events.
The most common early symptom[7] is intermittent claudication[1]. Claudication is defined as pain, cramping, numbness or fatigue in the calf, thighs or hips during walking or activity, that typically gets better with rest. Other visible signs include loss of hair on lower legs[3], shiny or discoloured skin, and leg weakness[1] or numbness. Some might also observe slow-growing toenails, and sores[1] or small wounds that take very long to heal.
At advanced stages, patients can suffer from gangrene, and slow-healing wounds and ulcers[5] since poor circulation can slow down the body’s healing. This can aggravate further and result in tissue loss[8]or in even more severe cases, require limb amputation[8]. Intermittent claudication or pain can also morph into a constant burning pain[5] even while at rest, indicating critical limb ischaemia[7] wherein the blood flow to the limb is significantly restricted.
If you are over 50 years of age[1], and have any of the common risk factors including diabetes[1], smoking, obesity[9], high blood pressure, high cholesterol, or a family history[1], of the disease, you must absolutely seek medical help at the first sign of symptoms.
Impacts on daily Life
People with leg pain often restrict walking[2], to avoid the pain, which leads to reduced functional capacity and further mobility loss.
The quality of life can deteriorate further[2] as symptoms progress, and depression and anxiety[10] have been reported among many patients. Patients might struggle with helplessness and loss of independence[6] as the disease progresses, further affecting their mental and emotional state.
People suffering from PAD might also feel fear, uncertainty[8], and discomfort regarding social situations and jobs[8], further impacting their social life and self-perception.
Managing PAD in Daily Life
Early intervention is extremely important, especially when symptoms are mild and the disease has not progressed significantly. Timely detection can increase the chances of better outcomes like improved walking, less pain, and better quality of life. Conversely, delayed diagnosis can greatly increase the chance of amputations later[8], which can add social and economic burdens[9] on families.
PAD can be managed, and you can reclaim control over your life and movement. Following a healthy lifestyle is key to keeping PAD at bay. However, if you have PAD, then seeking medical help for symptoms is the first step, followed by lifestyle management based on medical advice.
Managing diet and weight[9], and giving up smoking[9] are critical lifestyle changes. Managing stress[1], getting plenty of good sleep[1], as well managing diabetes, cholesterol, and blood pressure[1] are equally important.
Medical professionals might recommend a supervised exercise programme[11]to minimise discomfort while maximising movement for your improvement. Depending on the severity of the condition, the doctor might prescribe medication[11] as well.
Key takeaways for people
Peripheral Artery Disease often begins silently, but recognizing early warning signs can make a significant difference in the outcomes. Recurring leg pain during walking is one of the first and most common signs that must not be ignored, and may indicate reduced blood flow to the limbs, which can severely affect mobility and quality of life later on.
Awareness is key to making informed decisions. Many individuals are likely to dismiss leg pain as normal aging, delaying medical attention, and missing opportunities for treatment. Patient awareness[8] can significantly change PAD outcomes by allowing them to make the best choices for their health.
It is thus, extremely important to follow a healthy lifestyle, equip yourself with knowledge from verified sources, and always seek medical help when in doubt. While prevention may be better than cure in most cases, early diagnosis and intervention are extremely vital to managing PAD effectively and preserving quality of life.
References
- https://www.mayoclinic.org/diseases-conditions/peripheral-artery-disease/symptoms-causes/syc-20350557
- https://doi.org/10.1038/s41598-024-80387-1
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7948906/
- https://www.cdc.gov/heart-disease/about/peripheral-arterial-disease.html
- https://www.ncbi.nlm.nih.gov/books/NBK430745/
- https://doi.org/10.1371/journal.pone.0207456
- https://www.nhlbi.nih.gov/health/peripheral-artery-disease/symptoms
- https://doi.org/10.1016/j.jvn.2025.02.002
- https://doi.org/10.1161/CIR.0000000000001153
- https://doi.org/10.1016/j.avsg.2024.01.028
- https://www.mayoclinic.org/diseases-conditions/peripheral-artery-disease/diagnosis-treatment/drc-20350563