What Is Restenosis in Peripheral Artery Disease? Causes and Symptoms
Introduction
If you or someone close to you has been treated for Peripheral Artery Disease (PAD), you may hear doctors mention the term restenosis. It can sound worrying, especially if you believed the treatment had already fixed the problem.
Restenosis means that an artery narrows again after treatment. This blog explains restenosis in PAD, what it is, why it occurs, and the signs to watch for.
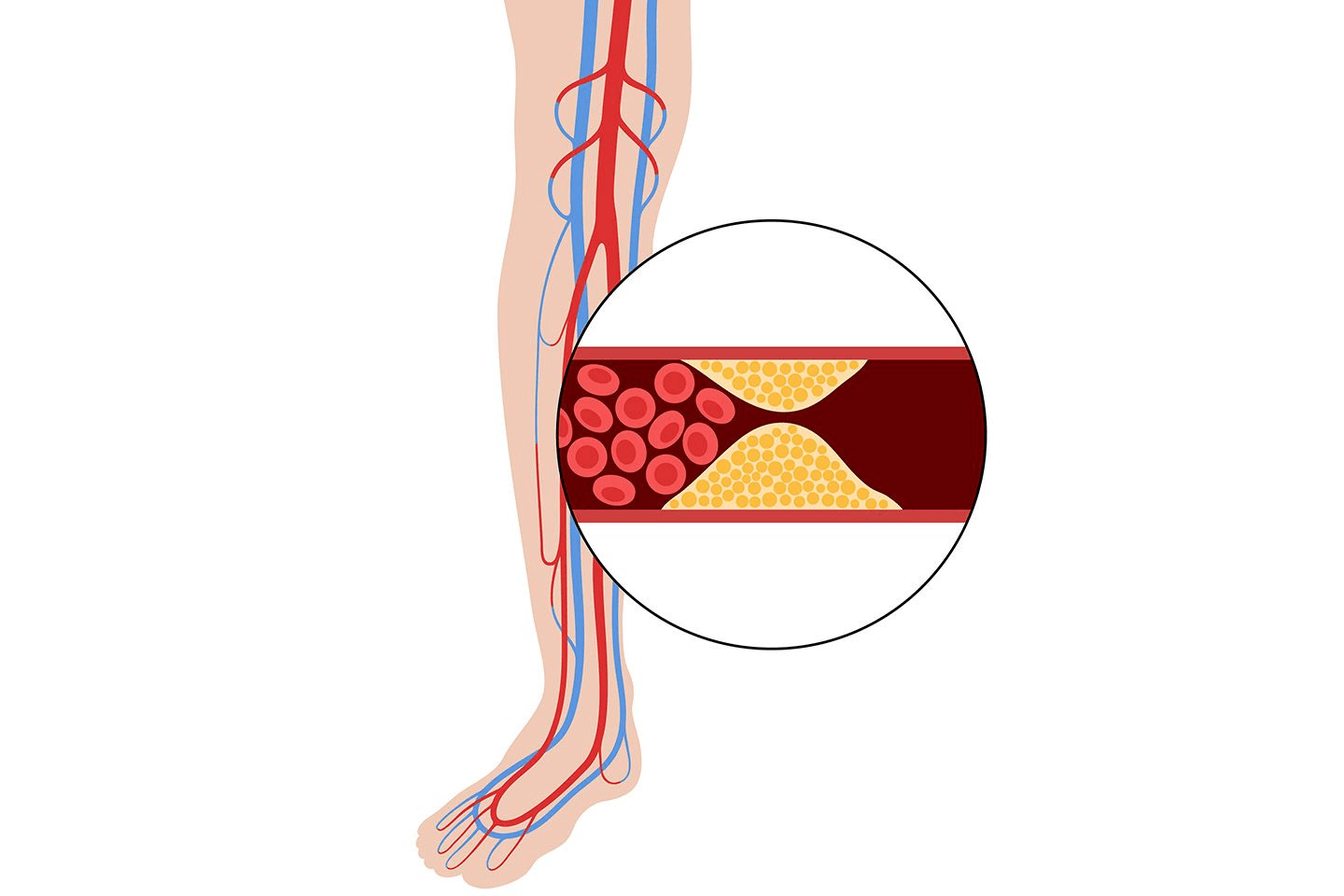
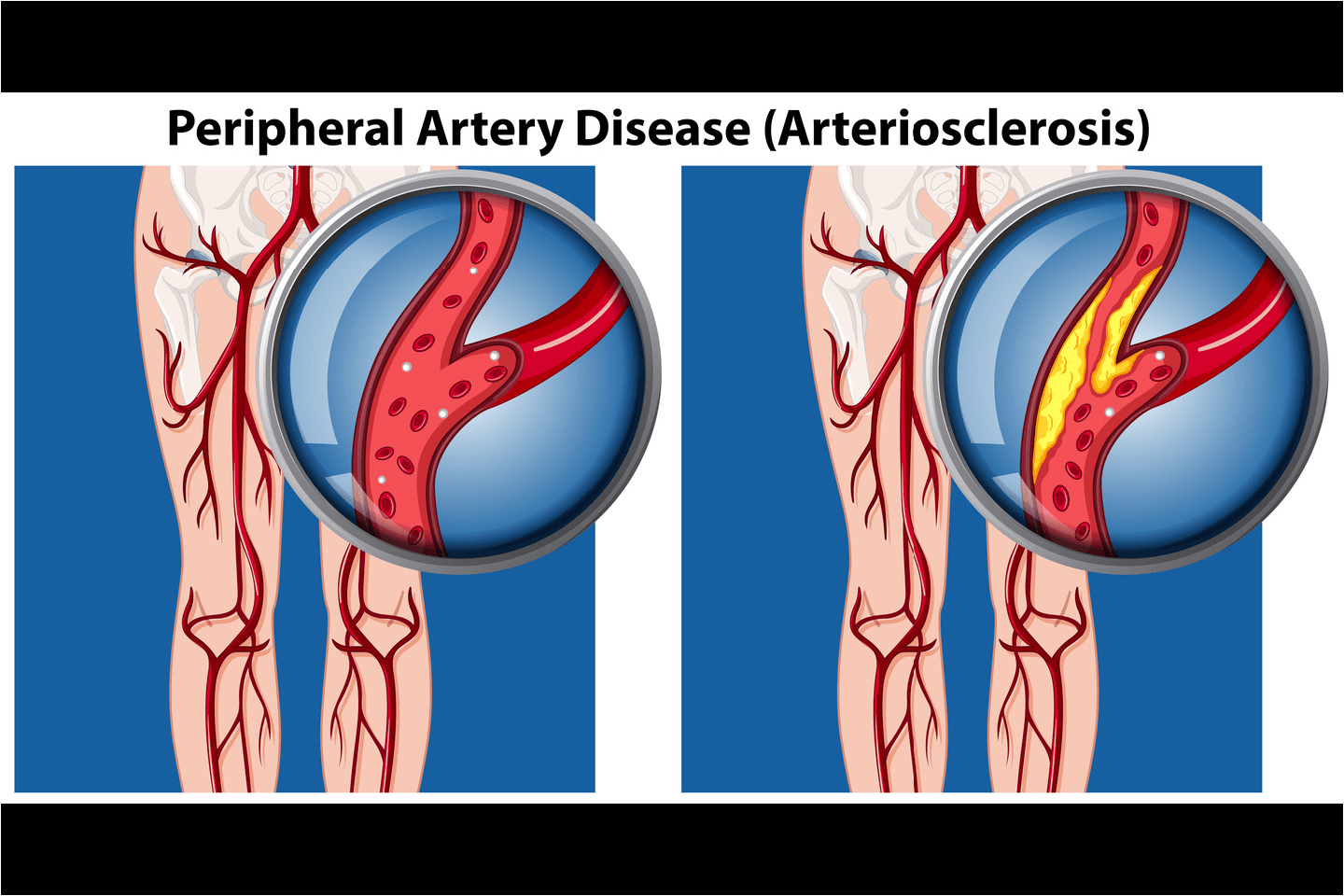
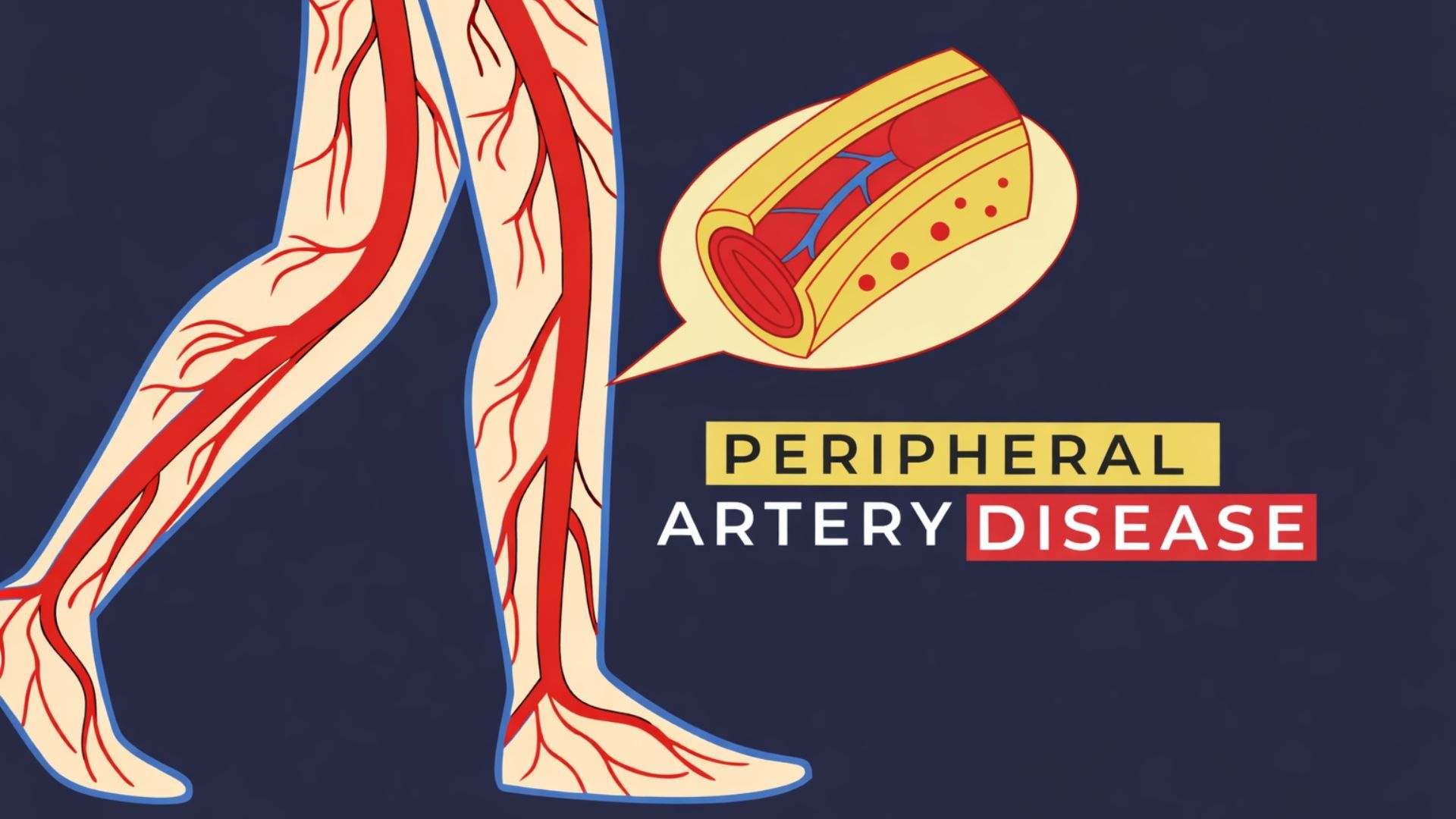
Understanding Peripheral Artery Disease
Peripheral Artery Disease affects blood flow to the peripheries, i.e., the legs and arms. It affects more than 200 million people around the world.[1]
In PAD:
Plaques are fatty deposits that build up on the walls of the arteries
Arteries become narrow and stiff
Blood struggles to reach muscles properly
This reduced blood flow often affects the legs because they are farthest from the heart. These are some common signs of PAD that one experiences:
Leg pain while walking
Coldness in the feet or toes
Slow-healing wounds
Tired or heavy legs
PAD usually develops slowly and may go unnoticed in the early stages.
What Is Restenosis?
Restenosis means re-narrowing of an artery after treatment. It can occur after three to six months,[2] after procedures such as:
Balloon angioplasty
Stent placement
Other minimally invasive artery-opening treatments
You can think of it like:
A blocked road is cleared. After the road is cleared, the traffic flows well for some time. Over months, the road narrows again due to repairs or debris. In the body, this "debris" is tissue growth or renewed plaque inside the artery.
Why Restenosis Can Occur?
After an artery is treated, the body tries to heal the area. Sometimes, this healing process becomes excessive. Common reasons restenosis develops may be that:
Scar tissue formation on the walls of the artery
Inflammation caused by vessel injury during treatment
Smooth muscle cell growth along artery walls
Plaque starts to rebuild on the walls over time
When you scrape your skin, a small scar forms. A similar process can happen on the walls of the arteries, but scar tissue can narrow the space for blood flow. Restenosis may often develop within:
3 to 6 months after treatment
Sometimes later, depending on risk factors
Who May Be More Likely to Experience Restenosis?
Not everyone with PAD develops restenosis. Certain factors increase the likelihood. Higher risk may be seen in people who:
Have a history of smoking
Have diabetes
Have high cholesterol
Have high blood pressure
Have long or severely blocked arteries
Have had repeated artery procedures
However, your lifestyle can also play a role. If you have limited physical activity, do not follow the care instructions given and diet, and also if you are irregular with taking medication. Understanding these risks helps patients and doctors plan better long-term care.
Common Symptoms of Restenosis
Symptoms of restenosis are often similar to PAD symptoms and may gradually return after treatment. Here is what you should keep an eye on:
Leg pain when you are walking that improves with rest
Cramping in calves, thighs, or hips
Cold or numb feet
Weak pulse in the legs
Fatigue in the legs during daily activities
The symptoms may appear slowly, be milder at first and also worsen over time if untreated. Some people may not notice symptoms immediately, which is why follow-up checks are important.
How is Restenosis Diagnosed?
Doctors do not rely only on symptoms to detect restenosis. They will usually use a combination of diagnostic methods, which may include:
Physical examination to check pulses
Ankle-Brachial Index (ABI) test
Doppler ultrasound of the peripheral arteries.
CT angiography or MR angiography
Catheter-based angiography in selected cases
What do doctors look for during follow-ups?
Reduced blood flow
Narrowed artery segments
Changes compared to earlier scans
These tests help decide whether further treatment is needed.
Treatment Approaches and Role of Medical Devices
The doctor will suggest treatment based on the severity of restenosis, symptoms, and the patient's overall health. The treatment options may include:
Medication adjustments
Supervised exercise programmes
Repeat angioplasty
Use of advanced stents or drug-based technologies
In selected PAD cases, clinicians may use advanced vascular stent technologies designed to support long-term vessel patency. Meril Life develops interventional solutions that aim to:
Support controlled vessel healing
Reduce excessive tissue growth
Maintain improved blood flow
These solutions are chosen based on clinical judgement and individual patient needs.
Why It's Important to Monitor PAD After Treatment?
PAD treatment does not end once a procedure is done. One study stated that 12.5% people experienced restenosis.[3] You will visit your doctor for regular monitoring, as it helps:
Detect restenosis early
Prevent symptom worsening
Reduce the risk of ulcers or infections
Maintain mobility and quality of life
Follow-up care usually includes:
Routine clinical visits
Imaging when needed
Medication review
Lifestyle guidance
With early detection, management becomes simpler and more effective.
When to Seek Medical Advice?
You should contact your doctor promptly if you notice:
Return of leg pain after earlier improvement
New difficulty walking short distances
Non-healing foot wounds[1]
Sudden coldness or colour change in toes
Increasing numbness or weakness
Do not ignore symptoms, assuming they are "normal ageing". Early action can prevent complications.
Conclusion
Restenosis in Peripheral Artery Disease can feel discouraging, but it is a known and manageable part of vascular care. It does not mean your treatment was unsuccessful.
By understanding why restenosis occurs, recognising symptoms early, and attending regular follow-ups, you can protect your mobility and long-term health. With the right medical guidance and lifestyle care, many people continue to live active lives after PAD treatment.