7 types of Contraception Method for Females to Avoid Pregnancy
Introduction to Contraceptive Methods
Multiple types of contraception methods are available currently. However, all the types are not suitable for all users. Selection of the most applicable method of contraception for family planning and birth control, best suited for each couple, depends on multiple factors including the user’s general well-being, age and gender, frequency of sexual relationships and partners, desire to conceive in the future, as well as family history of reproductive health problems. Dual protection from the simultaneous risk for HIV and other STDs also should be considered, while selecting a method of contraception.
Long-acting Reversible Contraception (LARC) Methods
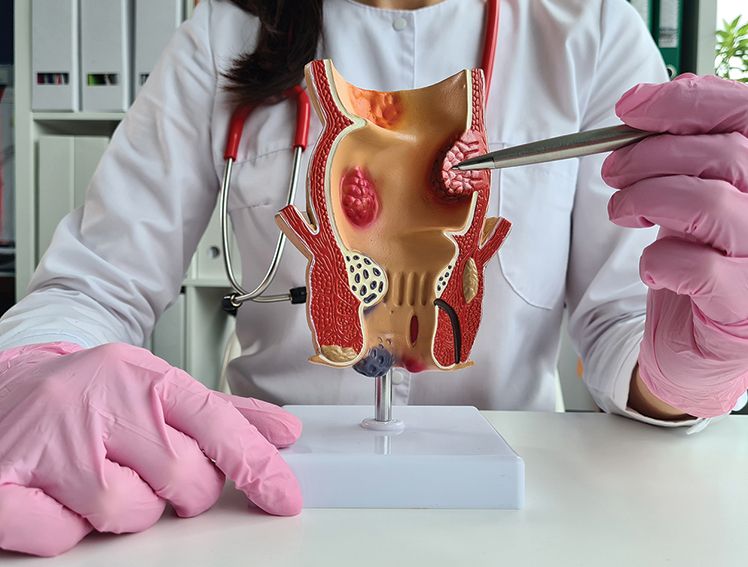
Intrauterine Device Implantation
An intrauterine device (IUD), also referred as IUS (intrauterine system), is a tiny device, bearing a T-shape, that is introduced into the uterus of the females for prevention of pregnancy. The gynecologist inserts the device. An IUD is equipped to stay in position and function effectively for multiple years (up to 10 years or more), altogether. After the recommended duration, or when the woman desires to become pregnant, the gynecologist can easily remove the device.
There are 2 types of IUDs available for contraception
- Hormonal IUD: These IUDs releases levonorgestrel (a progestin hormone) in minute quantities into the uterus, over multiple years. Levonorgestrel leads to thickening of the cervical mucus, preventing sperm from reaching or fertilizing the egg. It also weakens the uterine lining, and may stop the ovaries from releasing eggs. A hormonal IUD’s failure rate is less than 1%; but, a small percentage of women may encounter expulsion of the device and need re-insertion. It is suggested that these IUDs can preserve their effectiveness up to a year past their period of recommended use. The current method also effectively treats heavy menstrual bleeding as the hormone frequently reduces or removes uterine bleeding.
- Copper IUD: Copper IUD or Copper-T primarily works by disrupting sperm mobility and damaging sperm. It acts as a spermicide within the uterus. It increases levels of copper ions, prostaglandins, and white blood cells within the uterine and tubal fluids. Increased ions inhibit sperm mobility and viability, preventing sperm from traveling through the cervical mucus. The failure rate of Copper-T is similar to that of hormonal/levonorgestrel IUD. However, it is not recommended for use in women who are suspected to be pregnant, suffer from pelvic infections, have cervical or uterine malignancy, unexplained bleeding from the vagina or have uterine perforations.
Implantable Rods
These flexible devices are of the size of a matchstick, manufactured from plastic. These devices are surgically placed under the skin of the woman's upper arm. Comparable to IUDs, this method has a failure rate of <1%. The device releases a progestin and can be effective in preventing pregnancy for up to 5 years.
Hormonal Methods
Short-Acting Hormonal Methods
Hormonal methods of birth control use hormones to control or halt ovulation and prevent pregnancy. Ovulation is the physiological process where the ovary releases an egg, making it accessible for fertilization. Introduction of hormones into the body can be done through varied routes. These methods can prevent ovulation conditional to the types of hormones used; thickening cervical mucus, which helps preventing sperm from reaching the egg; or thinning the lining of the uterus. Health care providers recommend and observe hormonal contraceptives. Short-acting hormonal methods are highly effective as long as used perfectly, but in usual cases, they have a range of failure rates.Injectable birth control: This method involves injecting a progestin called depot medroxyprogesterone acetate [DMPA], in the arm or bums once every 3 months. Majority of patients using injectable birth control should eat a diet rich in calcium and vitamin D or take vitamin supplements while using this medication, as this method of birth control can cause a temporary loss of bone density, particularly in adolescents. However, this bone loss is generally temporary and can be reclaimed after discontinuing use of DMPA.
Progestin-only pills (POPs): A woman needs to take one pill daily, preferably at the exact time every day. POPs may delay ovulation or sperm function. POPs thicken cervical mucus, increasing difficulty for sperm to enter the fallopian tube. POPs change the normal cyclical changes in the uterine lining and may result in unscheduled or breakthrough bleeding. These hormones do not appear to increase risk of blood clots.
Combined Hormonal Methods
Combined hormonal methods contain ethinyl estradiol (a synthetic estrogen) and a progestin combination. These agents work by preventing ovulation and thickening cervical mucus. The combined estrogen/progestin drugs can be delivered in various forms. However, these combinations are associated with some medical risks, like blood clot formation, triggered by the presence of synthetic estrogen in these products. These risks are not evident in progestin-only products. Your doctor can guide you to select the most suitable contraceptive in your case depending on the individual’s risk factors.Combined oral contraceptives (COCs, "the pill"): COCs contain a synthetic estrogen and a progestin, which works through inhibition of ovulation. Multiple oral contraceptives are present, and your doctor helps to define which type best meets an individual’s needs.
Contraceptive patch: It is a thin, plastic patch that is attached to the skin and releases hormones through the skin into the blood. The patch is placed on the lower abdomen, bums, outer arm, or upper body.
Vaginal ring: The ring is thin and flexible tool, approximately 2 inches in diameter. It consists of a combination of ethinyl estradiol and a progestin. The ring is inserted into the vagina, where it continuously discharges hormones for 3 weeks. The woman needs to remove one ring every fourth week and re-insert a new ring, 7 days later. It is associated with certain risks, similar to COCs. These vaginal rings may not be suggested for women with certain co-morbidities, such as hypertension, heart disease, or some cancer types.
Barrier Methods
Barrier methods are changeable and may be used for women who cannot use hormonal methods of contraception. They are designed to prevent sperm from entering the uterus. Failure rates for barrier methods differ depending on the method.
Types of barrier methods that do not need a doctor’s visit include the following:
Male condoms: Condom is a thin cover that is worn on the penis to gather sperm and prevent it from entering the woman's body during intercourse. Male condoms are generally made of latex or polyurethane. These condoms reduce the risk of spreading sexually transmitted diseases (STDs). Condoms are equipped for a single use.
Female condoms: These condoms are thin, flexible plastic pouches. A part of the condom is inserted into a woman's vagina before intercourse to prevent sperm from entering the uterus. Additionally, these condoms also reduce the risk of STDs. These condoms are also meant for single use.
Contraceptive sponges: These are soft, disposable, spermicide-filled foam sponges. They are inserted into the vagina before intercourse. They help prevent sperm’s entry in the uterus, and the spermicide present in the foam also kills the sperm cells. The sponge should be left in place for at least 6 hours after intercourse and should not be present for more than 30 hours.
- A spermicide kills sperm cells: It can be used alone or in combination with a diaphragm or cervical cap. The most common spermicidal agent is a chemical called nonoxynol-9 (N-9). It is available in multiple strengths and forms, including foam, jelly, cream, suppository, and film. A spermicide should be inserted into the vagina close to the uterus no more than 30 minutes prior to intercourse and left in place for 6 to 8 hours after intercourse to prevent pregnancy. Spermicides do not prevent the STD transmission and may lead to allergic reactions or inflammation of vaginal tissues.
Methods that require a doctor’s visit include the following:
Diaphragms: Diaphragms are shallow, flexible cups composed from latex or soft rubber, inserted into the vagina prior to an intercourse, preventing sperm’s entry into the uterus. Preferably, spermicidal cream or jelly should be used with a diaphragm. The diaphragm should remain in place for 6 to 8 hours after intercourse to prevent pregnancy, but it should be removed within 24 hours. Conventional latex diaphragms must be of the correct size to function properly, and only a doctor can define the proper fit. A diaphragm should be replaced after 1 or 2 years.
- Cervical caps: These are similar to diaphragms but are smaller and more rigid. The cervical cap is a thin silicone cup, inserted into the vagina before intercourse to block sperm from entering the uterus. The cervical cap should be also be used with spermicidal cream or jelly. The cap must remain in place for 6 to 8 hours after intercourse to prevent pregnancy, but it should be removed within 48 hours. Cervical caps are available in variable sizes, and a doctor defines the best fit. With proper care, a cervical cap can be used for 2 years before replacement.
Emergency Contraception
Emergency contraception can be used after unprotected intercourse or if a condom breaks.
Copper IUD: The copper IUD is the most effective method of emergency contraception. The device needs to be inserted within 120 hours of unprotected intercourse. The method is nearly 100% effective at preventing pregnancy and possesses the additional benefit of contraception for a prolonged duration of up to 10 years. There are very few contraindications associated with a copper IUD, and there are also no concerns related to weight or obesity associated with the effectiveness of the method.
- Emergency contraceptive pills (ECPs): ECPs are oral hormonal pills, consumed either as a single dose or two doses 12 hours apart, meant for use in case of unprotected intercourse. If taken before ovulation, the pills can postpone or stop ovulation for at least 5 days to allow the sperm to become inactive. They also cause thickening of cervical mucus and may interfere with sperm function. ECPs should be taken as soon as possible after semen exposure and should not be used as a regular contraceptive method. Pregnancy can occur if the pills are taken after ovulation or if the woman has unprotected sex in the same cycle.
Sterilization
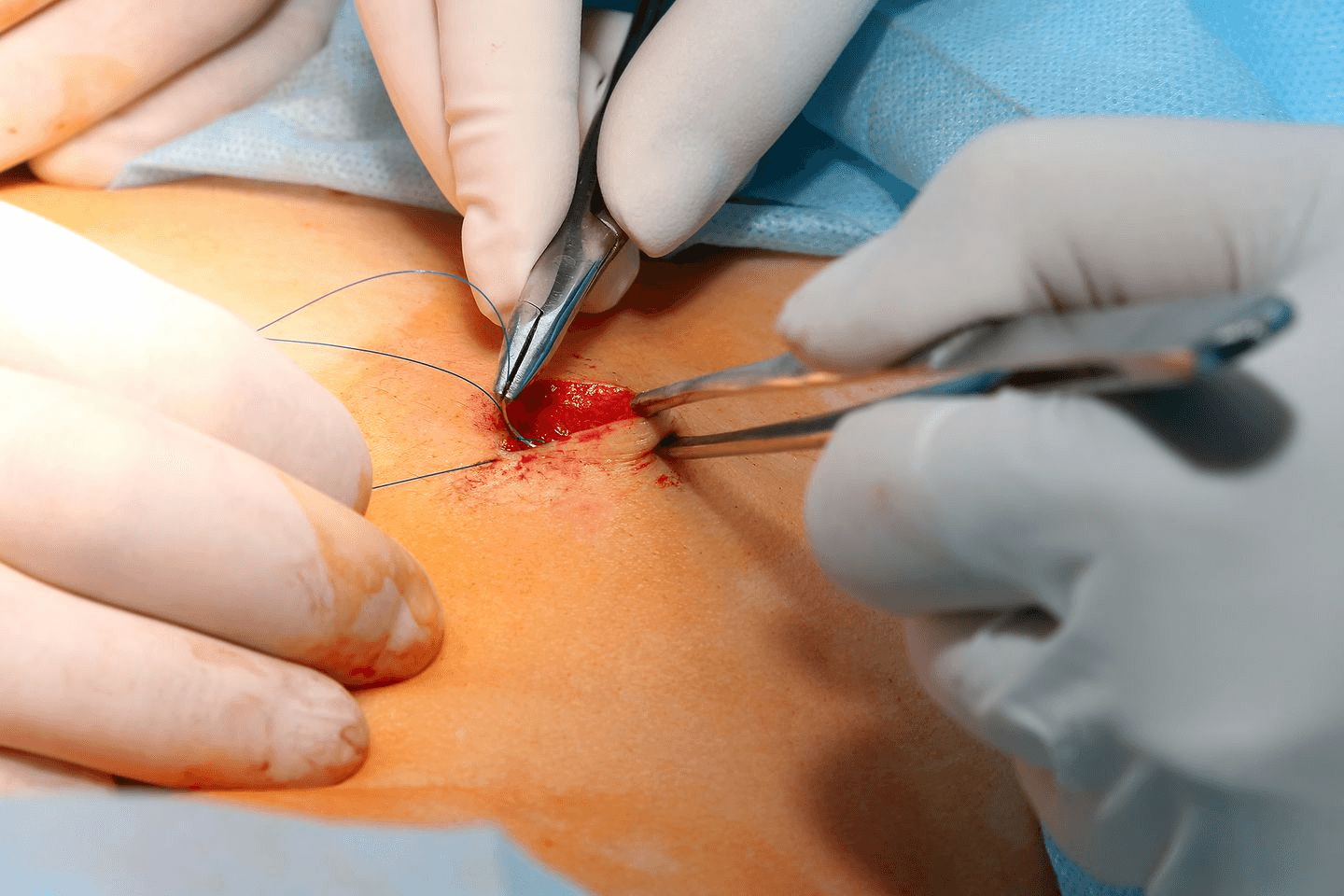
Sterilization is a permanent form of birth control that either prevents a woman from getting pregnant or prevents a man from releasing sperm. A doctor/surgeon must perform the sterilization procedure, which generally involves a surgical procedure. These procedures usually are non-reversible.
A sterilization implant is a nonsurgical method for permanently blocking the fallopian tubes. A doctor enters a thin tube through the vagina and into the uterus to place a soft, flexible insert into each fallopian tube. No incisions are necessary. During the next 3 months, scar tissue forms around the inserts and blocks the fallopian tubes so that sperm cannot reach an egg. After 3 months, the doctor conducts tests to ensure that scar tissue has fully blocked the fallopian tubes. A backup method of contraception is used until the tests show that the tubes are fully blocked.
Tubal ligation (female sterilization) is a surgical procedure in which a doctor cuts, ties, or seals the fallopian tubes, blocking the path between the ovaries and the uterus. The sperm cannot reach the egg for fertilization, and the egg cannot reach the uterus.
- Vasectomy (male sterilization) is a surgical procedure that cuts, closes, or blocks the vas deferens, obstructing the path between the testes and the The sperm cannot leave the testes and cannot reach the egg. It can take as long as 3 months for the procedure to be fully effective.
Fertility Awareness-Based Methods
Knowing your monthly fertility pattern can assist you to get pregnant or avoid getting pregnant. Your fertility pattern is the number of days in the month when you are able to get pregnant, days when you are infertile, and days when fertility is unlikely, but possible. If you have a regular menstrual cycle, you have about nine or more fertile days each month. If you do not want to get pregnant, you should not have sex on the days you are fertile, or you use a barrier method of birth control on those days. However, range of typical use failure rates reaches to as high as 23%