Peripheral Artery Disease Treatment: Stents, BTK Scaffolds & Other Options
Introduction
Peripheral Artery Disease (PAD) treatment has evolved remarkably over the years, offering patients hope and improved quality of life. From simple balloon procedures to advanced stent technology and now bioresorbable scaffolds, options continue to expand. Among these, innovative solutions like the BTK bioresorbable scaffold are shaping the future of below-the-knee (BTK) artery treatment.
This article explains PAD, its treatment options, and how next-generation devices are redefining care for people with narrowed or blocked leg arteries.
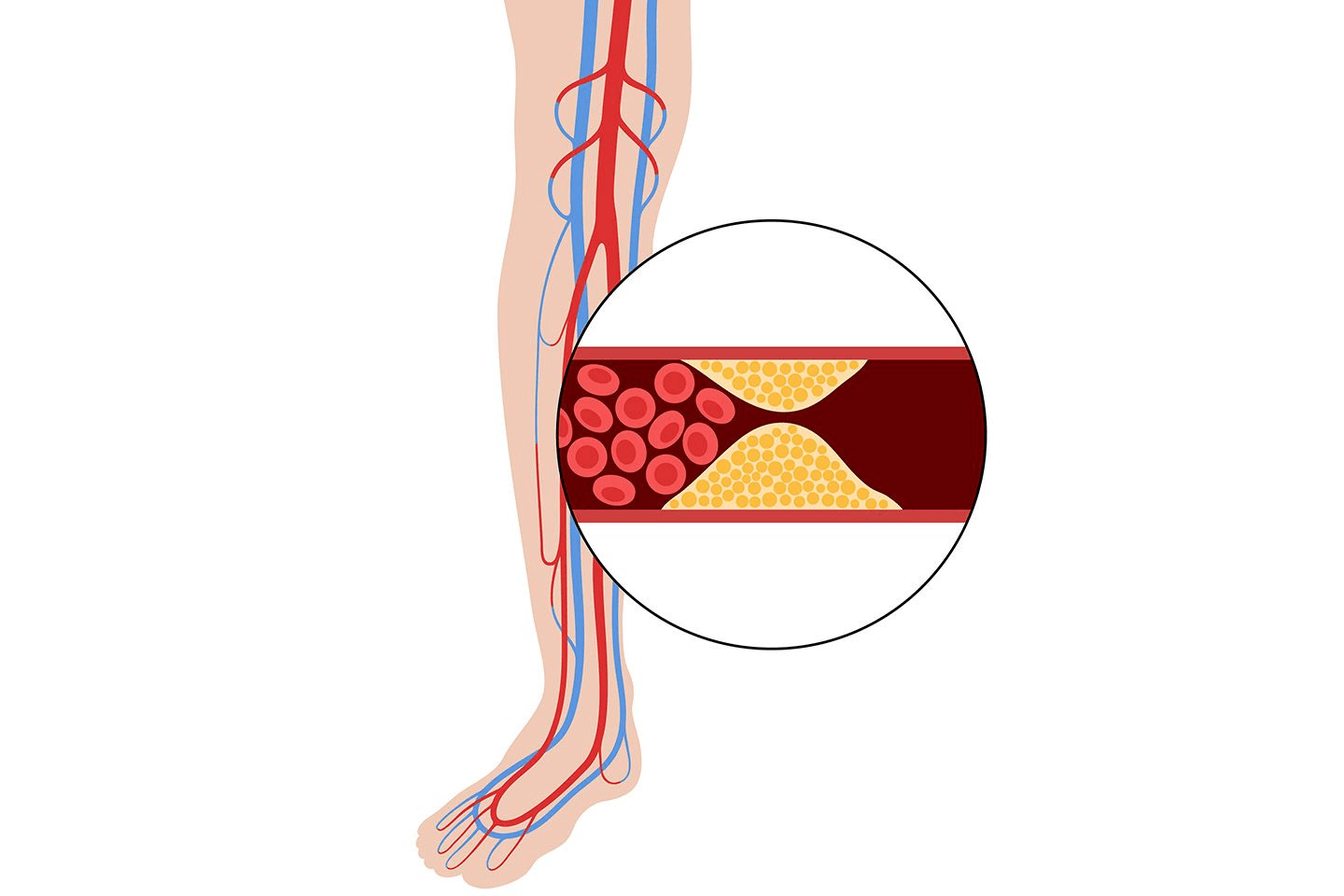
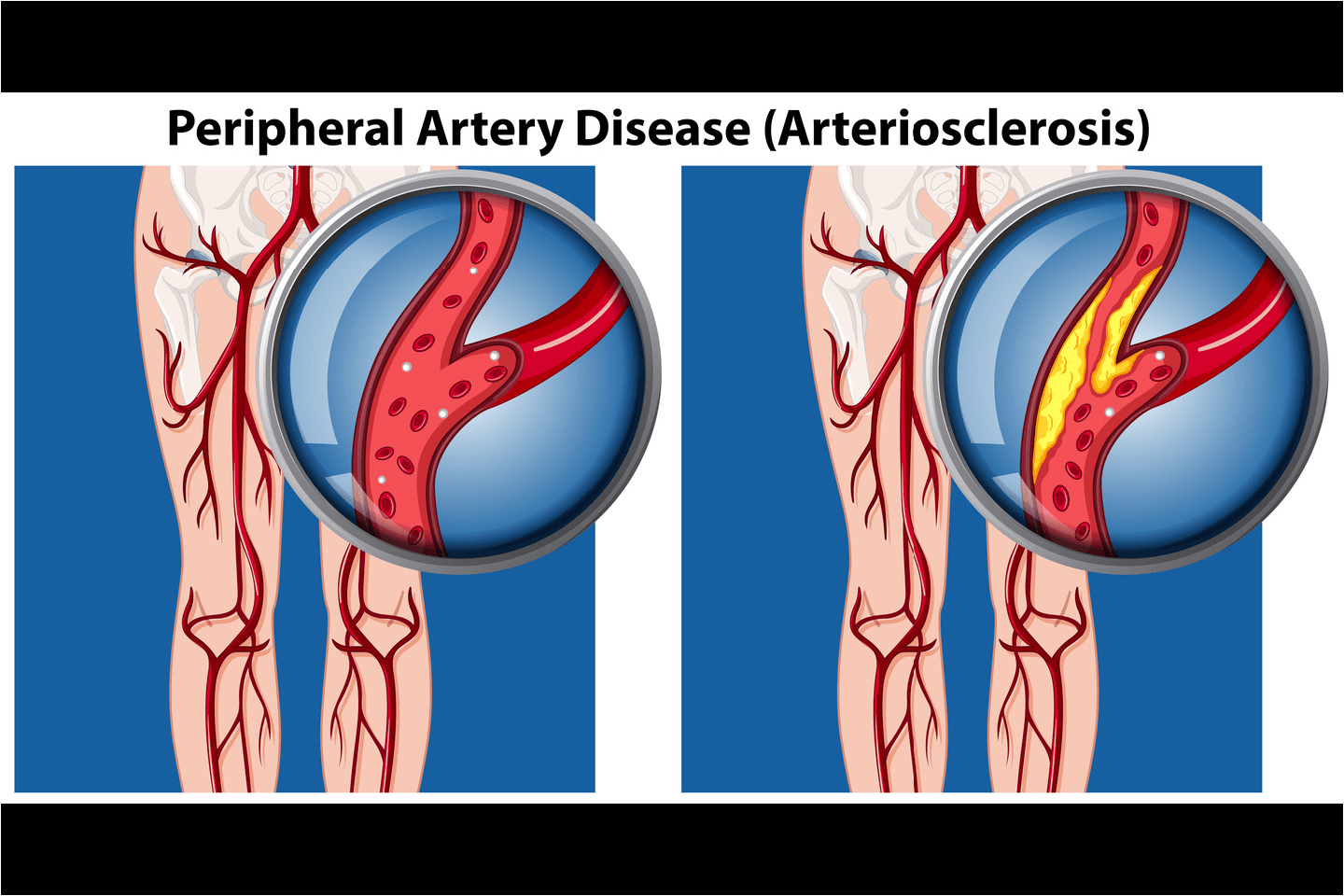
Understanding Peripheral Artery Disease (PAD)
Peripheral Artery Disease is a condition of the heart where arteries that carry blood to the limbs are narrowed due to plaque build-up. It can reduce blood flow, especially to the legs and feet, leading to pain, fatigue, or even non-healing wounds.
What is PAD in simple terms? It is like a "traffic jam" in your leg arteries that slows down oxygen delivery to muscles and tissues.
Symptoms and Risk Factors of PAD
PAD often develops silently. However, some signs should not be ignored:
Cramping or pain in the legs while walking (intermittent claudication)
Cold or pale feet
Slow-healing sores on toes or feet
Numbness or weakness in the legs
In severe cases, gangrene (tissue death)
Common risk factors include:
Diabetes
Smoking
High cholesterol
High blood pressure
Age above 50
Family history of cardiovascular disease[1]
When you know early, you can make lifestyle changes that will help prevent PAD from progressing.
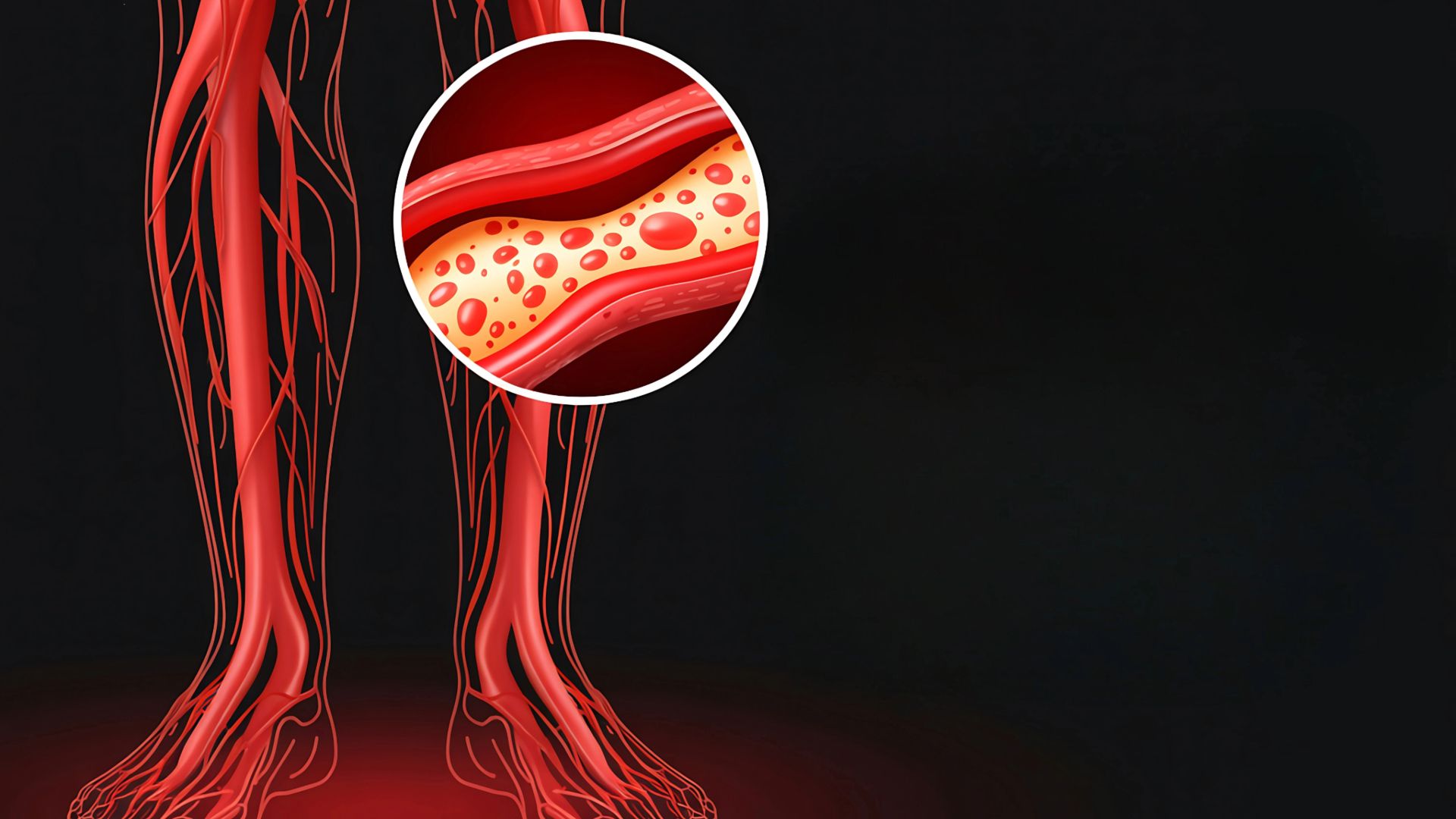
Why Below-the-Knee (BTK) Arteries Are Challenging
BTK arteries are smaller, more delicate, and prone to calcification. Treating blockages in these vessels is complex because:
The arteries are thin and fragile
Blood flow restoration must be precise
Conventional stents may not adapt well to constant leg movement
For patients with critical limb ischemia (CLI), BTK blockages can lead to chronic wounds and an increased risk of amputation, making effective and durable treatment essential.
Traditional PAD Treatment Options
Balloon Angioplasty (POBA)
Percutaneous transluminal angioplasty, or balloon angioplasty, is often the first step in treating PAD. A small balloon is inserted into the narrowed artery and inflated to widen it.
Advantages:
Minimally invasive
Quick recovery
Immediate blood flow improvement
Limitations:
The artery may narrow again (restenosis)
No long-term structural support
Metallic Stents and Their Limitations
Metallic stents were introduced to overcome restenosis. These tiny wire mesh tubes hold arteries open after angioplasty.
However, challenges remain:
Permanent metal presence may limit future treatment
Stent fractures can occur due to limb movement
May not suit small BTK arteries
Treatment Type | Purpose | Limitations |
Balloon Angioplasty | Opens narrowed artery | May re-narrow |
Metallic Stent | Provides structural support | Can fracture or block small arteries |
Bioresorbable Scaffold | Temporary support and drug release | Under evaluation but promising |
The Need for Innovation in BTK Interventions
Treating BTK arteries requires technology that supports the artery temporarily but doesn't stay forever. This is where bioresorbable scaffolds have emerged as a breakthrough, addressing the limitations of both balloons and permanent stents.
Bioresorbable Scaffolds in PAD
A bioresorbable scaffold (BRS) is a next-generation device that provides temporary support to the artery and slowly dissolves once healing is complete. Unlike metal stents, these scaffolds leave no permanent implant behind.[2]
Think of it as a "temporary cast" for your artery; it holds it open until the vessel heals, then safely disappears.
How They Work in BTK Arteries
A balloon delivers the scaffold into the blocked artery.
Once placed, it releases a drug (usually sirolimus) that prevents tissue growth.
Over time, the scaffold dissolves naturally, leaving behind a healthy, open artery.
Advantages over Permanent Implants
Natural healing: The artery regains flexibility once the scaffold dissolves.
Future-friendly: Allows repeat treatment if needed.
Reduced inflammation: No permanent metal means fewer long-term complications.
Drug delivery: Helps reduce restenosis.
What is the Credence BTK?
Meril's Credence BTK is an advanced sirolimus-eluting bioresorbable scaffold designed specifically for below-the-knee arteries. It is representative of a step forward in treating critical limb ischemia and Peripheral Artery Disease in small, complex vessels.
Key Highlights of Credence BTK
It is made from a specially engineered bioresorbable polymer.
It releases sirolimus to reduce the risk of artery narrowing.
It is designed to restore your blood flow while promoting vessel healing.
It is completely absorbed over time, leaving no metal behind.
This innovation supports Meril's vision of developing life-changing technologies for patients worldwide, particularly those suffering from severe PAD or limb-threatening conditions.
Benefits of BTK Scaffolds in PAD Treatment
Bioresorbable scaffolds have several advantages over traditional methods:
1. Temporary support, lasting results
They stabilise the artery during healing and then dissolve, ensuring the vessel remains flexible.
2. Drug delivery for long-term success
The sirolimus coating helps reduce the risk of re-narrowing (restenosis).
3. Reduced complications
No permanent metal means a lower risk of fracture or chronic inflammation.
4. Improved patient comfort
The absence of a long-term implant can make future procedures easier if needed.
5. Better outcomes in critical limb ischaemia
Improved blood flow helps in wound healing, reducing the risk of amputation in severe PAD cases.
The Future of PAD Treatment
The field of PAD treatment is evolving rapidly. As the medical field evolves, so do the medical technologies; the focus is shifting from merely opening blocked arteries to restoring natural vessel function.
Future therapies will likely combine:
Drug-eluting balloons for quick plaque reduction
Next-generation bioresorbable scaffolds for temporary yet effective support
Personalised treatment planning is done by using imaging and AI-based mapping
Meril's commitment to innovation and patient-centric design places it at the forefront of this transformation, with Credence BTK representing a significant step towards a "leave nothing behind" approach.
Conclusion
Peripheral Artery Disease can significantly impact daily life, but timely diagnosis and modern treatments help make a difference. While traditional stents and angioplasty have saved countless limbs, technologies are paving the way for safer, more durable, and future-ready solutions. By promoting natural healing and long-term artery health, bioresorbable scaffolds may well become the gold standard for below-the-knee PAD treatment.
FAQs
1. What causes Peripheral Artery Disease (PAD)?
PAD occurs when fatty deposits (plaque) build up in the walls of arteries, which reduces blood flow to the limbs.
2. How is PAD diagnosed?
Doctors use tests like an ankle-brachial index (ABI), Doppler ultrasound, or angiography to detect blockages.
3. What is the recovery time after PAD treatment?
Most minimally invasive PAD treatments allow recovery within a few days, depending on the severity of the disease.
4. How long does a bioresorbable scaffold stay in the body?
A scaffold like Credence BTK typically dissolves within months after the artery has healed.
5. Can PAD return after treatment?
Yes, if lifestyle risk factors persist. Regular follow-ups, healthy habits, and medication can help prevent recurrence.