Colorectal cancer (colon cancer)
Colorectal cancer starts when healthy cells shift and develop out of control in the lining of the colon or rectum, forming a mass called a tumor. A tumor may be benign or cancerous. A cancerous tumor is malignant, which means it can spread to other parts of the body and develop. A benign tumor means the tumor is capable of developing but is not going to spread. Such modifications typically take years to make. The changes can be caused by both genetic and environmental influences. When a person has an unusual inherited syndrome, however, changes can occur in months or years.

Anatomy of the colon and rectum
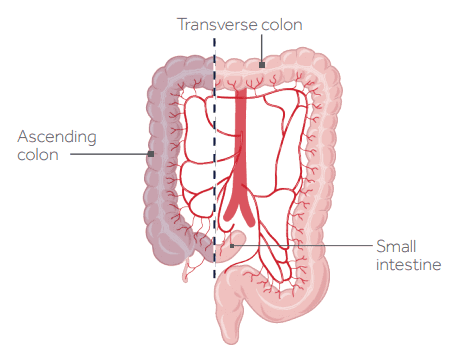
The large intestine, which plays an important part in the body's capacity to handle waste, is made up of the colon and rectum. The first 5 to 6 feet of the large intestine are formed by the colon and the rectum makes up the last 6 inches, finishing at the anus. There are 5 parts in the colon and rectum. The ascending colon is the part from a pouch called the cecum that spreads. The cecum is the beginning of the large intestine; it's on the right side of the abdomen, through which the small intestine empties.
The tip of the belly is crossed by the transverse colon. Down the left foot, the descending colon takes waste. Finally, a few more inches, down to the rectum, the sigmoid colon at the bottom takes waste. Waste, through the anus, exits the body.
Most common type of cancer of the gastrointestinal tract
It is the most prevalent form of gastrointestinal tract cancer, and a significant cause of death and sickness worldwide. In the abdominal cavity, the major intestine is located, and can be thought of as having two spaces - the intraperitoneal area and the retroperitoneal space.
Gastrointestinal tract are composed of four layers
Four layers of the gastrointestinal tract consist of
The first section of the duodenum, both the small intestines, the transverse colon, the sigmoid colon, and the rectum are in the intraperitoneal area; the distal duodenum, the ascending colon, the descending colon, and the anal canal are located in the retroperitoneal space. Thus, between the intraperitoneal and retroperitoneal spaces, the large intestines basically weave back and forth. Now, four layers are made of the walls of the gastrointestinal tract.
The outermost layer is the named serosa for the intraperitoneal parts, and the adventitia for the retroperitoneal parts.
The muscular layer, which contracts to transfer food across the intestine, is next. After that is the submucosa, which consists of a dense layer of tissue that contains blood vessels, lymphatics, and nerves. And finally, there’s the inner lining of the intestine called the mucosa; which surrounds the lumen of the gastrointestinal tract, and comes into direct contact with digested food.
The mucosa has invaginations called intestinal glands or colonic crypts, and it’s lined with large cells that are specialized in absorption. Most colorectal carcinomas are adenocarcinomas, meaning that they arise from the cells lining the intestinal glands.
Most cases of colorectal tumors happen because of sporadic mutations, but a small number are caused by known genetic mutations that run in a person’s family. An example of this is the adenomatous polyposis coli gene, or APC gene, which is a tumor suppressor gene.
Normally, the APC protein identifies when a cell is accumulating a lot of mutations and forces it to undergo apoptosis, or programmed cell death.
But when the APC gene is mutated, the mutated bowel cells don’t die, and instead some start dividing uncontrollably, giving rise to polyps. Over time, these polyps might accumulate more mutations in other tumor suppressor genes like the K-ras gene or the p53 gene, and ultimately it might might become a malignant tumor – meaning that the cells might be able to invade neighboring tissues.
Another well known example are genetic mutations in DNA repair genes which help fix up mutations in cellular DNA. When they’re out of action - cells accumulate mutations and over time can develop into polyps and eventually adenocarcinomas.
So, broadly speaking, adenocarcinomas are the malignant evolution of polyps, and polyps arise when cells start dividing faster than usual. There are many different types of polyps, and some are more prone to become malignant; those are called pre-malignant or neoplastic polyps.
These pre-malignant polyps can be classified into adenomatous and serrated, according to how they look under the microscope. Typically, adenomatous polyps have an APC mutation and the cells look like normal colonic mucosa cells, whereas serrated polyps have defects in DNA repair genes and have a saw-tooth appearance.
Stages of Colon Cancer
When tumors become cancerous, they can be categorized into stages.
Stage 0 is carcinoma in situ, meaning that the tumor has not grown beyond the mucosa.
Stage 1 is when the tumor has grown beyond the mucosa, but has not spread to lymph nodes or distant organs.
Stage 2 is when the tumor has invaded the whole colonic or rectal wall, and may have reached nearby organs or tissues, but still hasn’t spread to lymph nodes or distant organs.
Stage 3 is when the tumor had spread to lymph nodes, but still hasn’t spread to distant organs.
Finally, stage 4 is metastatic, meaning that the tumor has spread to distant organs.
The most common site of metastasis for colon cancer is the liver, and for rectal cancer it’s the lungs.
There are some non-modifiable risk factors for colorectal cancer like being an elderly male and having inflammatory bowel disease, but there are some modifiable risk factors as well, like smoking cigarettes, eating a lot of red meat, not eating a lot of fiber, and being obese.
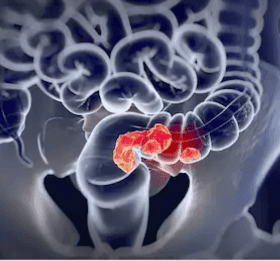
Colorectal cancer are also also associated with specific disorders like familial adenomatous polyposis and hereditary nonpolyposis colorectal cancer. Initially, colorectal carcinoma is often asymptomatic, but as the disease progresses, symptoms can develop depending on the tumor’s location. In general, cancers in the ascending or right colon expand outward beyond the mucosal surface, which may cause vague abdominal pain and weight loss.
These tumors usually do not cause bowel obstruction, which means they may develop very large before causing symptoms, and it also means that a late diagnosis is always made. This tumors can ulcerate and bleed, and bleeding can lead to anemia caused by iron deficiency over time.
Tumors located on the descending or left colon are generally infiltrating masses, meaning that they tend to be ring-shaped masses that involve the whole circumferenLARce of the colonic wall.
This causes lumen narrowing, referred to as napkin-ring constriction, so symptoms of bowel obstruction typically happen early on. Bowel obstruction can cause colicky abdominal pain, and blood-streaked stools, called hematochezia.
source image:Colorectal Cancer Alliance
What is Low Anterior Resection? (LAR)
LAR is a procedure that is done for the treatment of rectal cancer. The section of your rectum along with the cancer will be separated during LAR surgery. It would reconnect the remaining section of your rectum to your colon. When you heal from your surgery, you will be able to get bowel movements (poop) as normal.
Different Technique of LAR Surgery?
When 1 long incision is made on your abdomen, this is called open surgery.The cancer section of your rectum will be thoroughly eliminated from the incision.
The cancer section of your rectum will be thoroughly eliminated from the incision. This is considered minimally invasive surgery, where many minor incisions are made on the abdomen. To extract the cancer, small surgical instruments and a film camera will be inserted into the incisions. To aid with the procedure, some surgeons use a robotic system.
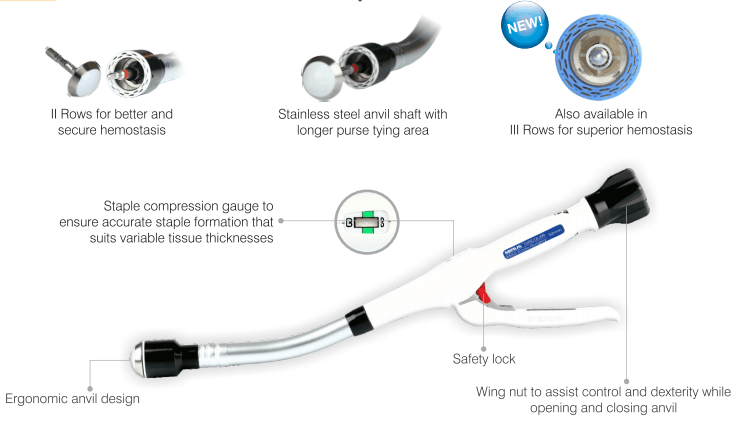
Once the cancer section of your rectum is removed, tiny metal staples or sutures will reconnect the remaining part of your rectum to your colon (stitches). An anastomosis is called the site where the 2 ends are reconnected.
LAR surgery usually takes about 4 hours.
What are the Symptoms of colon cancer
· A continuous change in your bowel patterns, like diarrhea or constipation, or a change in your stool's quality
· Rectal bleeding in the feces or blood
· Persistent discomfort in the belly, such as cramps, gas or pain
· A sense that the stomach is not absolutely empty
· Fatigue or exhaustion
· An unexplained reduction of weight
What causes colon cancer
In general, as healthy cells in the colon undergo modifications (mutations) in their DNA, colon cancer starts. The DNA of a cell includes a set of instructions which tell a cell what to do. In an ordered manner, healthy cells develop and split to keep the body functioning normally. But cells begin to divide when the DNA of a cell is destroyed and becomes cancerous, even when new cells are not required. They form a tumor as the cells multiply. The cancer cells may multiply over time to invade and kill nearby normal tissue. And cancerous cells may migrate to other areas of the body and produce deposits there (metastasis).
What are the Risk factors involved in Colorectal cancer
Factors that can raise the risk of cancer of the colon include:
Older age. It is possible to diagnose colon cancer at any age, although the majority of patients with colon cancer are older than 50. Colon cancer rates have been rising among people younger than 50, but doctors aren't know why.
Afro-American race. There is a higher chance of colon cancer for African-Americans than for people of other races.
A personal history of polyps or colorectal cancer. You have a higher chance of bowel cancer in the future if you have either had colon cancer or noncancerous colon polyps.
Inflammatory bowel disorders. Your chance of colon cancer can be elevated by chronic inflammatory diseases of the colon, such as ulcerative colitis and Crohn's disease.
Inherited syndromes that raise the risk of colon cancer. Your chance of colon cancer can be greatly elevated by certain gene mutations inherited through generations of your family. Inherited genes are related to only a limited number of colon cancers.
Inherited genes are related to only a limited number of colon cancers. Family adenomatous polyposis (FAP) and Lynch syndrome, also known as genetic colorectal cancer without polyposis, are the most common inherited syndromes that raise the risk of colon cancer known as hereditary nonpolyposis colorectal cancer (HNPCC)
Colon cancer family history. When you have a blood relatives that has had the illness, you are more likely to develop colon cancer. Your chance is much higher if more than one family member has colon cancer or rectal cancer.
High-fat, low-fiber diet. A traditional Western diet, which is low in fibre and high in fat and calories, can be associated with colon cancer and rectal cancer. Research has had mixed results in this region. In persons who consume diets rich in red meat and processed meat, several studies have found an elevated risk of colon cancer.
A sedentary way of life. It is more likely that people who are inactive will develop colon cancer. Your chance of colon cancer can be decreased by doing daily physical exercise.
How Colon Cancer is Diagnosed
There are several Medical test which can diagnosed the cancer are below mention-
Barium Enema
Biopsy
Colonoscopy
Digital Rectal Exam
Sigmoidoscopy
Endoscopy
Colonoscopy- which is when a camera is inserted retrograde into the colon and rectum and to take pictures of abnormal looking polyps and a biopsy.
In addition, fecal occult blood testing is often done to look for evidence of gastrointestinal bleeding.
Typically, in colorectal cancer there’s an elevation in the tumor marker CEA, which is a glycoprotein involved in cell adhesion.
However, this is not a very specific finding. A barium enema can be useful as well. That’s where a liquid is injected into the rectum through a small tube, and an X ray is taken to look for abnormalities in the large intestines.
On a barium enema, a classic sign of colorectal cancer is the apple core sign, which shows the constriction of the lumen - most often in the descending colon. To identify colorectal cancer early, routine colonoscopy and fecal occult blood test can be done to look for neoplastic polyps or early carcinomas so that they can be removed at an early stage. This is particularly important for individuals with relatives with colorectal cancer and those with disorders like familial adenomatous polyposis and hereditary nonpolyposis colorectal cancer.
Disease Area: Rectum
Steps:
Access through separation of GI layers
Identification and mobilization of malignant area
Transection, Resection & Anastomosis
Treatment / Surgery for Colon Cancer
Treatment for colorectal cancer depends on the stage of the cancer. Early cancers that are confined to the wall of the colon are often surgically resected, and those that have spread to nearby lymph nodes are often treated with chemotherapy.
Unfortunately, metastatic cancers are typically incurable, but sometimes chemotherapy or surgery can be used to ease symptoms.
Surgery to remove more or half of the colon is called a colectomy. They also remove surrounding lymph nodes. It is termed a hemicolectomy, partial colectomy, or segmental resection if only half of the colon is removed. The surgeon removes the cancer section of the colon and a small part of the usual colon on either side. Learn More about MIRUS Circular stapler.