Obesity is described as having an excessive amount of body fat that develops when its amount is exceeded by the intake of fats for energy use. it's calculated as an index of body mass (BMI).

Causes of Obesity
A number of factors contribute to obesity, making it a complex health problem to tackle. It is called a combination of any or more of the following:
Excessive consumption of food
Lack of physical activity, as well as
Hereditary sensitivity
A few cases are mainly caused by genes, endocrine disorders, drugs, or mental illness. In general, evidence to support the belief that obese individuals eat little but gain weight because of a slow metabolism is not supported.
Body Mass Index:
The Body Mass Index (BMI) is a method of evaluating whether or not the weight of a person falls inside the healthy range. It is a good body fat indicator. BMI does not distinguish between muscle mass and body fat. Therefore, while they are not overweight or obese, body builders and individuals with muscle mass display a high BMI
Consequences of Obesity
Obesity is related to many serious physiological, psychological and social consequences, as listed below.
Following are the Physiological consequences of obesity
Type 2 Diabetes
High blood pressure
Heart disease
Gallbladder disease
Cancer (breast, uterine and colon cancer)
Digestive disorders (gastroesophageal reflux disease or GERD)
Breathing problems (asthma)
Problems with fertility and pregnancy
Urinary incontinence
Joint problems (arthritis)
Shorter life expectancy
Psychological and social consequences of obesity are:
Negative self-image
Social discrimination and isolation
Depression
Anxiety
BMI | Classification | Health Risk |
Under 18.5 | Underweight | Minimal |
18.5 - 24.9 | Normal Weight | Minimal |
25 - 29.9 | Overweight | Increased |
30 - 34.9 | Obese | High |
35 - 39.9 | Severely Obese | Very High |
40 and over | Morbidly Obese | Extremely High |
Obesity Treatment Options
Obesity treatment involve different surgical or non-surgical methods.
Non-Surgical Treatment
Nutrition
Non-surgical therapy primarily includes dietary counseling to improve the weight loss program, with or without the use of supplements. Nutrition control and supplements are the foundations of weight loss and are highly individualistic. A reasonable goal for weight loss is approximately 1.0 -1.5 kg/wk in the sense of a nutrition-based treatment program. The concept that the weight loss target must be individualized for each subject and should not be unilaterally based on the traditional weight-for-height diet norms is becoming increasingly apparent.
Lifestyle Changes
The best way to start your weight loss program is to know where your lifestyle routine goes wrong and adjust it in order that you still work the proper way towards weight loss.
In the long run, simply starving in the name of diet and gym won't help. They will give you an initial satisfactory loss of weight, but you tend to lose energy after a few months and become weak instead of losing weight. To focus on your diet and lose weight without much hard work, you just need to be smart.
Exercise
Eating well is only part of the fight when it comes to good and effective weight loss. By burning calories and building muscle, physical exercise will help you inch closer to your goal. That's not the only reason, however for making exercise part of your everyday life. Exercise also helps avoid many infections, reduces stress, and makes you feel better.
Surgical Treatment for Obesity
Surgery for weight loss has considered to be a successful method for treating morbid obesity. There are multiple options today, thanks to the continuous evolution of surgical principles, that allow both patients and surgeons to decide on the procedure of choice in line with their convenience.
Any of the surgical procedures carried out to treat obesity include the following:
Intragastric balloon
Gastric banding
Sleeve gastrectomy
Roux-en-Y gastric bypass
Mini Gastric Bypass
Other novel procedures
The biggest development in bariatric surgery is the use of laparoscopy to perform these procedures. The laparoscopic procedure is a minimally invasive procedure where small incisions are made to perform the surgery. Patients undergo the procedure with minimal pain and rapid recovery.
Indications
The reasons for obesity surgery are in line with internationally accepted guidelines,
People with BMI > 40 kg/m2
Patient how has BMI>35 with pronounced co-morbidities.
People with failed non-surgical attempts at weight reduction over a period of 1 year
People with absence of surgical contraindications or concomitant diseases
People with age group between 18 and 65 years
Contraindications
Bariatric surgery isn't recommended in patients with:
Inflammatory diseases like regional enteritis
Patient with Severe heart, lung or liver diseases
Patient who has history of auto immune diseases like scleroderma or systemic lupus erythematous
Patient with alcohol or white plague
Patient who are under the age of 18 years
Patient who are Pregnant
Patient with chronic pancreatitis (inflammation of the pancreas)
Presence of Infection.
Sleeve Gastrectomy
Sleeve gastrectomy is a surgery performed for the treatment of obesity, also named as vertical sleeve, gastric sleeve or tube gastrectomy. The procedure for treating severely obese patients with a high BMI of 40 and above is restrictive bariatric surgery
By minimizing the stomach size, it facilitates weight loss so that it holds only a small amount of food. This helps patients eat less without hindering the natural process of digestion. Sleeve gastrectomy is often performed in severely obese patients with a BMI of 60 or more as the first stage of a 2-stage operation. This is required to obtain a substantial amount of weight loss so that if appropriate, it is better for the patient to undergo a second bariatric surgery.
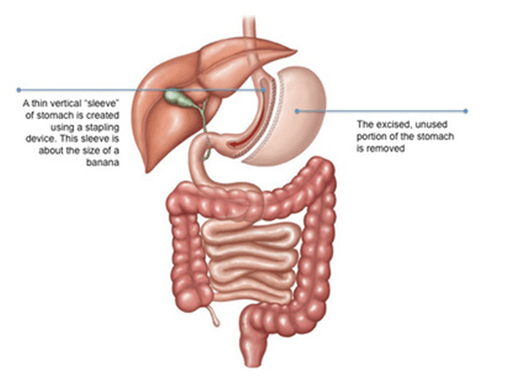
Sleeve Gastrectomy – Surgery
Under general anaesthesia, the procedure is performed. The surgeon makes 2 to 5 tiny abdominal incisions. A laparoscope is placed through one incision, a thin device with a light and a camera attached, allowing the surgeon to clearly see the internal organs on a monitor.
Via the other incisions, additional surgical instruments are inserted. Nearly 80 percent of the stomach will be removed by the surgeon. Stapling the remaining portion of the stomach forms a thin sleeve shaped like a banana. The incisions are closed at the end of the operation with sutures. It takes between 60 to 90 minutes to complete the entire process.
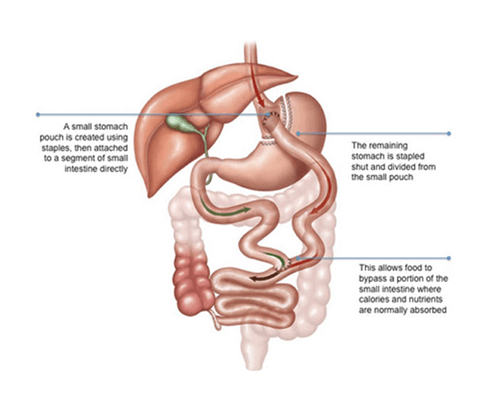
Roux-En-Y Gastric Bypass
For obese patients who have not been effective in losing weight by dieting, exercise and medication, gastric bypass is a way out for those. Gastric bypass also referred to as Roux-en-Y gastric bypass, is a bariatric or weight loss procedure. to get a good result, the surgeon uses a combination of restrictive and mal-absorptive techniques. To limit the quantity of food intake, staples are used to build a smaller stomach, and an oversized a part of the small intestine is bypassed to limit the nutrients and calories consumed.
It has been shown that gastric bypass surgery helps minimize obesity and associated diseases, including cardiovascular disease, high blood pressure, and type 2 diabetes particularly.
Surgery:
Under general anaesthesia, gastric bypass surgery is carried out. Several tiny incisions are made on your abdomen by your surgeon. A laparoscope is inserted into one of the incisions, a thin device with a light and a camera at the top, enabling the surgeon to clearly see the internal organs on a monitor. To execute the surgery, small surgical instruments are inserted through the other incisions.
The first step is to reduce the stomach's size so that it contains less food. By stapling, the upper portion of the stomach near the oesophagus is converted into a pouch. The second phase of the procedure includes the development of a bypass for food from of the new stomach pouch to flow. There is a division of the small intestine into upper and lower segments. The lower intestine segment is connected to the opening in the stomach pouch, forming what is known as the alimentary limb. The upper section of the small intestine which carries digestive juices from the remaining portion of the stomach is attached at the distal end of the roux limb. The roux limb which enables food to bypass the lower stomach, duodenum, and a portion of the small intestine. During the end of the procedure, the incisions are closed with sutures.
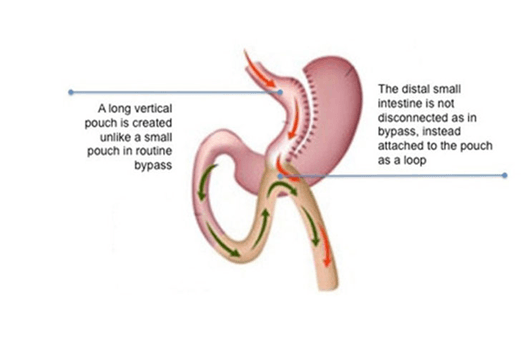
Mini Gastric Bypass
The Mini Gastric Bypass (MGB) is a short, simple, successful, reversible laparoscopic gastric bypass weight loss surgery. it's been recently renamed as one Anastomosis Gastric Bypass.
Mini Gastric Bypass Surgery
Under general anaesthesia, Mini Gastric bypass surgery is carried out. Several tiny incisions are made on your abdomen by your surgeon. A laparoscope is inserted into one of the incisions, a thin device with a light and a camera at the top, enabling the surgeon to clearly see the internal organs on a monitor. To execute the surgery, small surgical instruments are inserted through the other incisions.
The first step is to reduce the stomach's size so that it contains less food. By stapling, the stomach is transformed into a long slender pouch up to the antral section. The second phase of the procedure includes the development of a bypass for food from the new stomach pouch to flow. Depending on the surgeon and the metabolic state of the patient, a loop of small intestine ideally between 150 and 250 cm is selected for anastomosis. The middle part of the gut is connected to the opening in the intestine. stomach pouch creating what is referred to as the "omega loop". The loop allows the lower stomach, duodenum, and a part of the small intestine to be bypassed by food. The incisions are closed with sutures at the end of the operation.
Bariatric & Metabolic Surgical Devices
Tissue thickness presents a unique challenge when stapling laparoscopically. Endocutters are designed to mitigate the forces placed on them during firing based on the tissue thicknesses in order to provide consistent staple formation and transect intended tissues. However, as tissue thickness varies across the body, we need one solution across a broad range of tissue thicknesses, and simplifying the cartridge selection process with optimal compression has been a critical need for many surgeons.
Keeping in mind to eliminate human suffering Meril Endo surgery introduced MIRUS Linear cutter and Mirus Endoscopic Linear cutter with TRIO reloads. The MIRUS Endocutters are intended to use in minimally invasive surgical procedures for the transection, resection of tissues and creation of anastomosis in these procedures.
Mirus Endoscopic linear cutter and TRIO reloads are available in lengths 45mm & 60mm with three rows varied height staples to accommodate varied tissue thicknesses.
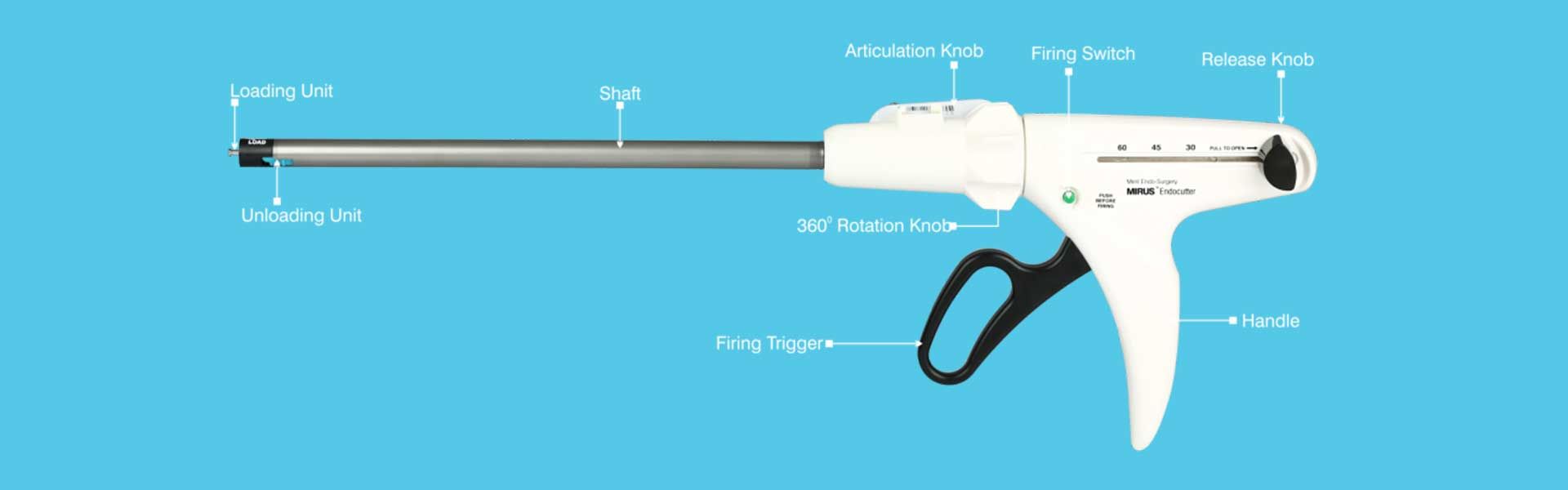
Benefits: Mirus Endoscopic linear cutter and TRIO reloads
Optimal Compression & Consistent staple formation gives superior hemostasis
Ease of handling facilitates better tissue manipulation
A new Knife gives a precise and smooth transection
Aids better transection, resection and creation of anastomosis
With the development of such different tools few surgeries have become really easy and less painful compared to open surgery such as Bariatric surgeries.
Endoscopic Linear cutters are commonly used to create a GIS anastomosis because of their ability to cut and staple simultaneously. In particular, they are almost indispensable in bariatric, gastric, and pouch surgery, surgeries in which complications lead to a high rate of morbidity and mortality. To minimize the incidence of anastomotic leakage and bleeding along with optimal tissue compression to create safer anastomosis MIRUS Endoscopic Cutter was launched. The new linear cutter provides some advantages to the surgeon. Its Varied Height staple feature accommodates various tissue thicknesses. This accommodation may be helpful in case of the absence of a suitable cartridge for the standard instrument for an operation.
