All you need to know about Percutaneous Coronary Interventions
Introduction
Heart disease is the leading cause of death around the world, making it essential to find and treat it early. It affects the heart and the blood vessels that supply blood throughout the body. When doctors find heart problems early, they can help you get better treatment and care. One of the most common types is coronary artery disease, which happens when the arteries that bring blood to your heart muscle become narrow or blocked. This narrowing is caused by a buildup of fatty deposits (called plaque) in the arteries. Indians have been reported to have the highest CAD rate, with rural areas having half the prevalence of urban areas in India. Asian Indians have approximately. 20% to 50% higher mortality associated with the disease compared to other populations. Effective control of their rising cases calls for proactive efforts in diagnosing and treating the disease. This blog will discuss the two treatment options for treating CAD, particularly Angioplasty, also called percutaneous coronary intervention (PCI).
Treatment Options for CAD
There are two main ways doctors can treat blocked heart arteries: bypass surgery and balloon angioplasty. Bypass surgery (also called CABG) is a highly invasive procedure where surgeons open the chest and create a new path around the blocked artery using a blood vessel from another part of the body, like the leg or chest. Balloon angioplasty (also called PCI or angioplasty) is a less invasive procedure that uses a thin tube inserted through a small puncture in the wrist or groin. The word 'percutaneous' simply means 'through the skin' - so this procedure works by going through the skin instead of requiring major surgery.
The clinical decision for the type of treatment option depends upon the heart team's evaluation of the patient's age, sex, coronary physiology, clinical anatomy, and complexity. CABG has been a standard treatment for patients with complex lesions, multiple blockages, or blockage of left main artery. However, PCI has been a preferred modality in permissible cases of CAD. With its non-surgical approach, minimal invasiveness, shorter hospital stays, and faster recovery, PCI has been gaining acceptance and expansion as a standard of care for patients with CAD.
History of Angioplasty or PCI
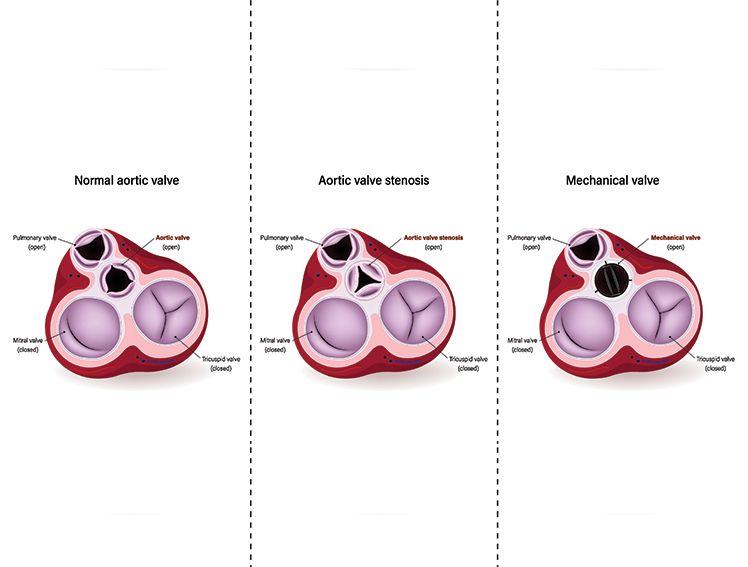
Intervention Cardiology has been evolving with technological advancements and the subsequent introduction of novel devices and new treatment therapies that aim to meet the challenges of the existing treatment options. It emerged as a discipline with the introduction of the first balloon angioplasty, the Plain Old Balloon Angioplasty (POBA). This first PCI has led to the foundation for treating cardiovascular diseases through minimal invasiveness. The advancement in this field is witnessed through the emergence of Bioresorbable Scaffolds (BRS), transcatheter aortic valve replacement procedure (TAVR), Transcatheter Mitral Valve Replacement (TMVR), 3D imaging, and Robotic-assisted PCI, enabling intervention cardiologists to treat more severe cardiovascular diseases and cater to the complex needs of the patients with comorbidities and other valvular complications with positive outcomes.
Various types of Angioplasties
From POBA to PCI using BRS, the journey of intervention cardiology has been remarkably evolving.
- Balloon Angioplasty
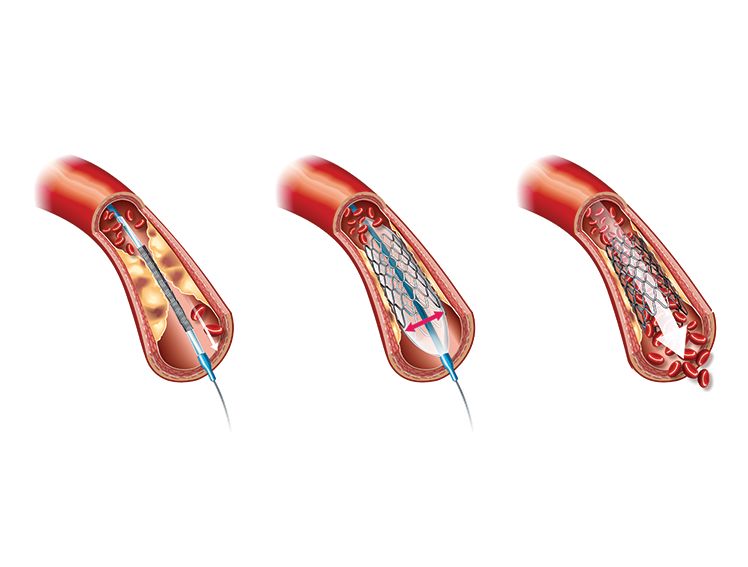
It is the basic procedure for treating CAD. The intervention cardiologist makes a small incision in the groin or arm to locate an artery for a catheter to pass. Through a sheath (a small tube inserted in the artery to keep it open), a catheter is passed along the artery and guided to the blocked coronary artery. A tiny balloon attached to the tip of the catheter is guided to the site of the plaque through the blood vessel. Once at the correct position, the balloon is inflated, pushing the plaque to the side of the artery's walls, allowing the blood to flow uninterrupted. Once the plaque is removed, using a small amount of contrast dye, the intervention cardiologist will check the opened artery to ensure proper and improved blood flow. The balloon is deflated, the surgical instruments are removed, and the incision is closed. - Angioplasty With Stents
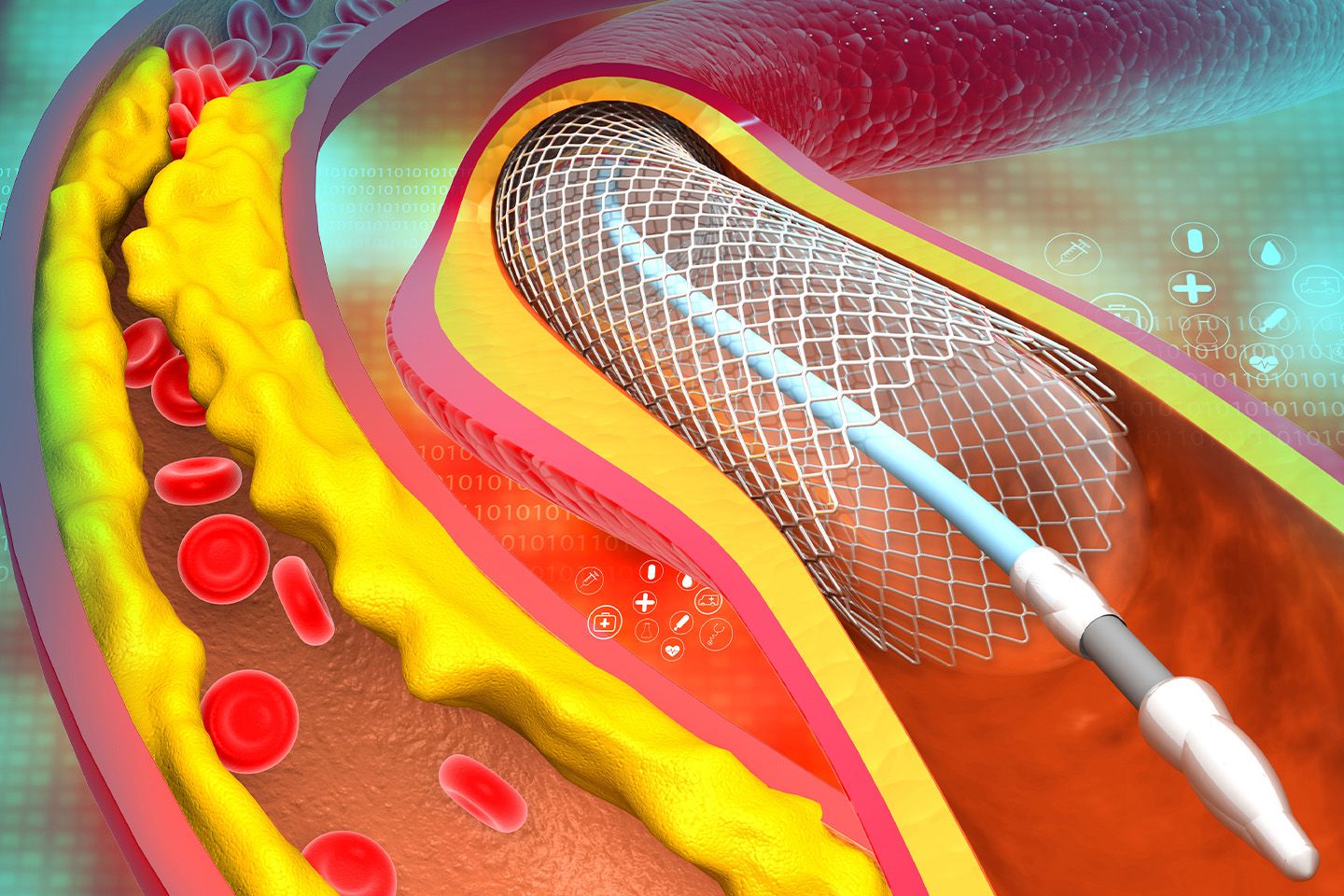
In the case of coronary stenting, the balloon at the tip of the catheter has a stent attached. When the balloon is inflated to remove the plaque, the stent opens and gets properly adjusted in the arterial space created by removing the plaque. The stent holds the artery walls open, ensuring smooth blood flow. The balloon is removed along with the catheter and the sheath, and the incision is closed.
A stent is a small mesh of metal that keeps the artery open for uninterrupted blood to flow. The evolution of PCI has been through, in addition to other technological developments, advances in stent composition to overcome the challenges of the existing devices. There are three main types of stents:
- Bare metal stents are made of bare metal mesh, like tiny springs that prop open the artery.
- Drug-eluting stents are metal stents with a special coating that slowly releases medicine to prevent scar tissue from growing and re-blocking the artery.
- Bioresorbable stent (BRS), also called dissolving stents, are temporary supports made from materials that the body gradually absorbs over time, leaving no permanent device behind.
Risks and Benefits from PCI
Like any medical procedure, balloon angioplasty has some risks, but serious complications are uncommon. The most common risks include:
- Bleeding or infection at the spot where the thin tube was inserted (usually your wrist or groin) - this is typically mild and heals quickly.
- Blood clots can rarely form in the stent, which is why you'll take blood-thinning medication as prescribed.
- Re-narrowing of the treated artery can sometimes happen months later, but medicine-coated stents greatly reduce this risk. Your doctor will discuss your specific risks based on your health and the complexity of your blockage.
The acceptance of PCI as a mainstay treatment option for CAD can be attributed to the benefits derived from it in the form of-
- Minimal invasiveness
- Improved blood flow
- Reduced chest pain and shortness of breath
- Safer procedure with low risk for less complex cases
- Less operative time
- Shorter hospital stay
- Less scarring, pain, and recovery time
Angioplasty or PCI Procedure
Pre-Operative Procedure
- The patient is put on a sedative to help relax.
- The hair on the groin or arm, where the catheter is inserted, is removed, and the area is cleaned.
- For administering medicines, an Intravenous (IV) line is placed.
Oxygen level is tracked with a pulse oximeter clipped at the finger or ear. - The heart is monitored, placing electrodes on the patient's body.
During the Procedure.
- The patient is given local anaesthesia, either on the groin or the arm, from where the catheter is inserted.
- A contrast dye is injected once the catheter is at the surgical site to view the vessel blockage on the X-ray.
- A suitable Angioplasty stent is placed, and the procedure takes approximately an hour or three.
- Once completed, the catheter and other surgical devices are removed, and the incision is closed.
Post Operative Procedure
- The patient is under observation in the recovery room for a few hours.
- Post-operative pain and discomfort are taken care of through pain medication.
- The patient is advised to drink water and other fluids to flush out the dye.
- Depending on the patient's condition, the discharge from the hospital may be on the same day or the next.
Recovery
It takes a few weeks for most patients to return to their routine. However, it depends on the individual case. At the time of discharge from the hospital, the doctor will schedule the patient's follow-up appointments and advise on pain management through wound care, medications, and lifestyle changes through exercise, diet, and stress management to ensure proper healing and recovery. Some may need post-operative rehabilitation that helps and supports them in their recovery and healing. Patients may undergo specific diagnostic tests like X-rays, blood tests, and echocardiograms at regular intervals for a year after Angioplasty.
Meril’s Vascular Intervention Devices
Meril’s Vascular Intervention medical devices range from Balloon Catheter, Drug Eluting Stents (DES), Bioresorbable Scaffolds (BRS) to Transcatheter Aortic Valve Replacement System (TAVR). Meril’s products are used in more than 100 countries.
EVERMINE50 from Meril
EVERMINE50 from Meril is a breakthrough in DES. It comes with a hybrid cell stent design with open cells in the middle for side branch access and closed cells at the ends of the stent, ensuring optimal scaffolding and conformability. With an ultra-low strut thickness of 50μm, it promotes faster healing.
BIOMIMETM – Sirolimus Eluting Coronary Stent System
BIOMIME is a next-generation Sirolimus Eluting Coronary Stent with a novel hybrid design of closed cells at the ends and open cells at the middle. It has ultra-thin 65 µm strut thickness and biodegradable polymer-based DES for faster healing.
A Note from Meril
Angioplasty, or PCI, has been gaining increasing acceptance as a standard treatment of care for CAD patients due to its minimally invasive approach, lesser pain and discomfort, shorter hospital stays, and faster recovery. It is noted that the choice between CABG or PCI as the treatment option for CAD is weighed on various factors, including but not limited to the patient's age, sex, coronary physiology, clinical anatomy, and complexity. The decision of the interventional cardiologist is jointly arrived at after consulting his multidisciplinary medical team. Both treatment options aim to treat CAD effectively with positive patient outcomes.