BIORESORBABLE SCAFFOLDS - The New Age Dissolving Stents
Cardiovascular diseases (CVDs) are the leading cause of mortality and have a remarkably high prevalence in India with an increasing number of deaths due to CVDs in the younger population.¹ For the Indian population, the particular concerns regarding CVD are the early age of onset, rapid progression, and high death rate.
With this come the challenges to promoting cardiovascular health among the young population by understanding the socioeconomic, biological, and behavioural aspects of this age group.
After the clinical evaluation of the patients, Medical Management, Angioplasty or CABG (Bypass surgery) may be recommended to patients. Angioplasty is a less invasive and preferred modality for permissible cases than Open heart bypass surgery.
The advancement in interventional cardiology offers various treatment options for complications related to CAD, with PTCA in the mainstay. From the first balloon angioplasty performed more than 40 years ago to the present-day advent of the new age dissolving stents, the field of interventional cardiology has evolved significantly. In this blog, we will overview the two recommended interventions, the role of Bioresorbable Scaffolds (BRS) / Dissolving Stents and their advantage in post PTCA recovery, healing and restoring the physiological functions of the treated vessel.
What is Coronary Artery Bypass?
Coronary Artery Bypass, an open-heart surgery aims to treat the clogged passage of the artery through bypassing it, taking a new route with a new blood vessel taken from another part of the body. This new vessel is attached to the coronary artery creating a new path for the blood to flow around the diseased artery. This process of taking the new vessel from the body part and using it to divert the blood flow is known as grafting.
What is Angioplasty?
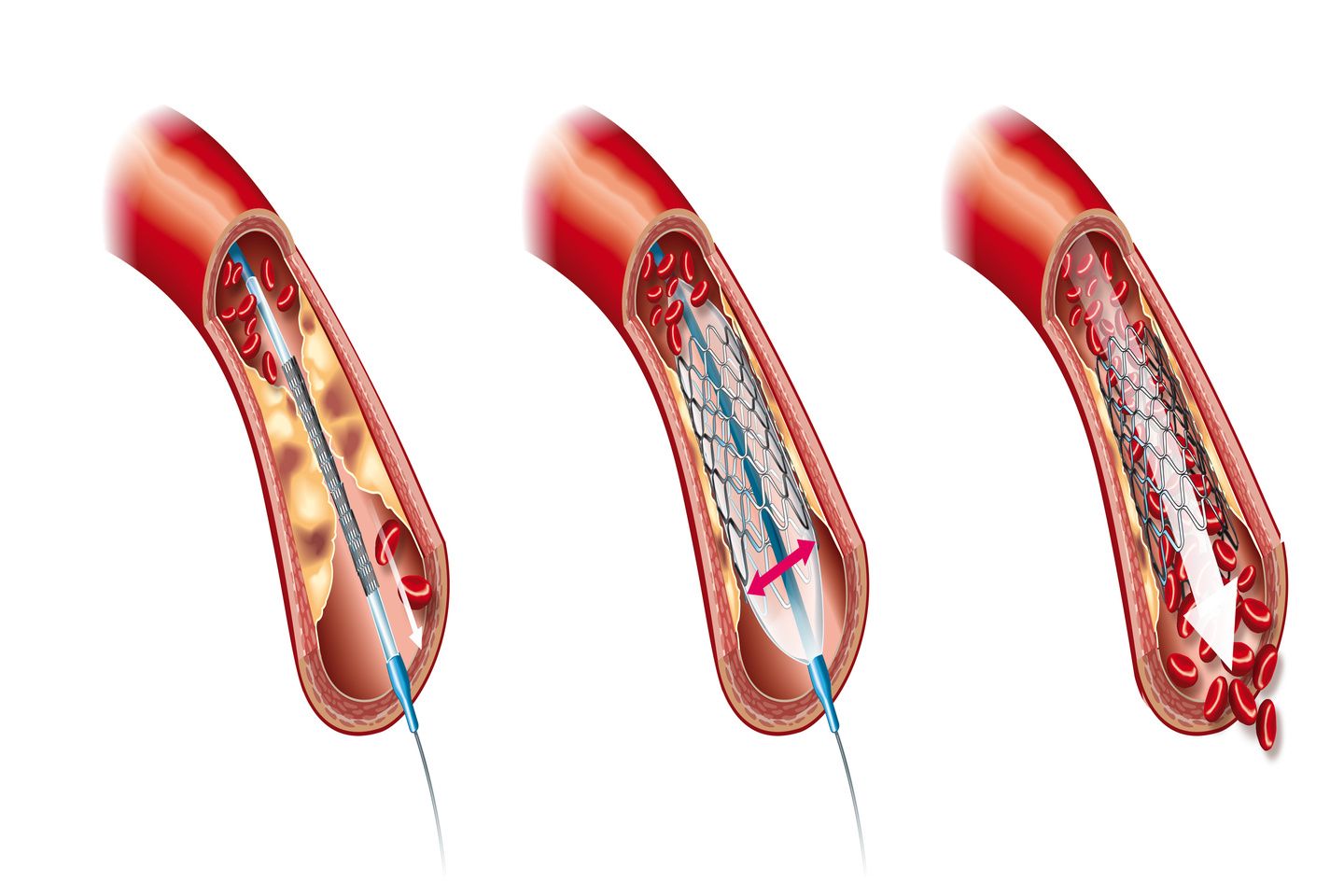
Angioplasty, also called Percutaneous Transluminal Coronary Angioplasty (PTCA) is a less invasive alternative treatment option to open the narrowed or clogged arteries resulting from atherosclerosis (accumulation of plaque inside the arteries) thus improving the blood supply through the arteries to the heart muscle. Angioplasty with or without stenting is a nonsurgical procedure to treat the clogged arteries.
Stents are expandable metallic wire mesh put inside the clogged arteries to open the artery and prevent narrowing. The use of various stents like the bare metal stents (thin metallic wire mesh without any coating and drug), the drug-eluting stents (metallic stents coated with medicine drug that is released directly in the treated arteries with the aim to reduce the re-growth of scar tissue), dissolving stents (stents that dissolve over a period of time leaving no residue inside the body as a temporary scaffold/support to the treated artery and designed to dissolve naturally once the healing is complete approximately in two to three years) has been ever evolving, with each subsequent evolution trying to seek solutions for the existing challenges faced by the current advancement.
Why Dissolving Stents?
The dawn of dissolving stents also called Bioresorbable Scaffolds (BRS) arose from the need for an alternative to reduce the long-term effect of metal stenting post (PTCA) and restore the vessels with temporary mechanical support. The bare metal stents and the drug-eluting stents with their permanent presence which cage the heart arteries carry certain risk of long-term adverse events. Approximately, 1.5% - 2% adverse events are reported every year with permanent stents.
BRS once completely absorbed, with its 'no residue' left in the body removes potential reasons for late adverse effects while preserving all the options for future re-interventions. This comes as a significant boon, especially for patients undergoing PTCA, using BRS at a young age. The scaffold undergoes three stages of degradation, starting from the 'rebuilt phase' where the scaffold acts like the drug-eluting stent providing deliverability, minimal acute recoil (decrease in stent area), high radial strength (force required to compress the stent), treating the lesion (injury to living tissue in the body or any organ) and restoring blood flow. In the 'revive phase' comprising three to six months post-implantation, there is a decline in the radial strength of the scaffold, followed by the discontinuance of the device to act as a scaffold in the 'rebuilt stage.'
BRS heralded as the latest advancement in the field of interventional cardiology.2 The significant advantage of BRS is that it provides temporary support to the vessel wall while simultaneously allowing the release of an anti-proliferative drug, helping the vessel to heal and restore its physiological function.
MeRes100™ from Meril
MeRes100™ is the next-generation BRS that provides fascinating characteristics not seen in the first-generation BRS, including a low strut thickness of 100 micron, a unique hybrid structure with closed cells at the edges and open cells in the middle, which provide optimal side-branch access, a wide range of sizes and diameters, and 3 radio-opaque marker couplets at the edges for precise deployment. MeRes100™ has demonstrated favorable and encouraging safety and efficacy outcomes data, which prove the results of no scaffold thrombosis 3 both in Indian and International patients.
Conclusion
Though BRS holds promise, the role of DES in treating CVDs cannot be undermined. DES remains the standard of treatment for patients undergoing PTCA since they have led to significant improvements in the clinical outcomes as compared to BMS. At present the available thin strut BRS has been currently studied in selected lesion and patient subset. DES is still good for the use of complex lesions.
To put it in a crux, the latest innovation in stent technology with the advent of the next generation thinner strut, BRS paves the way for metal-free or metal-less angioplasty.
References
Sreeniwas Kumar A, Sinha N. Cardiovascular disease in India: A 360 degree overview. Med J Armed Forces India. 2020 Jan;76(1):1-3. doi: 10.1016/j.mjafi.2019.12.005.
https://www.merillife.com/medical-devices/vascular-intervention/coronary/scaffold/bioresorbable-scaffold/meres100
Seth A et al., EuroIntervention 2019;15:1-9