The 3 Most common types of Fistula
Introduction
Fistulotomy is one of the most commonly used surgical procedures to treat fistulas. What are fistulas, you may ask? Two organs of your body may form a connection that could lead to the growth of abscess pockets. This growth is abnormal and is called a fistula. Fistulas can occur in any part of the body.
Unlike fistulectomy, which involves a surgical procedure to remove the abnormal growth or fistula, fistulotomy usually involves opening and draining the pockets.
Fistulas and fistulotomy may sound nasty and concerning, however, there is nothing to be worried about. Fistulotomy is a minor outpatient surgery, and you can be on your way home the same day of your surgery.
Before we delve into the fistulotomy procedure, let’s understand what causes a fistula to grow.
What is fistula?
A fistula has a connection or passageway between two organs, vessels, or surfaces that are not intended to be connected. These abnormal tunnels can happen anywhere in the body, allowing the fluids or other substances to jump between places they shouldn’t be. The fistulas would naturally appear congenitally, make their first occurrence from an injury, be a complication of surgery, or appear from a medical condition.
Fistulas may be anatomically classified as:
- Complete fistula: Features openings on both ends with a connecting tunnel
- Incomplete fistula: Contains only one external opening
- Open one side and close on the other — Blind fistula
Without treatment, incomplete and blind fistulas tend to evolve into complete fistulas, which may progress toward more serious complications over time.
What causes fistula
Multiple factors can cause fistula formation.
Common Causes:
- Abscess: Failure of an infection to heal properly
- Crohn’s disease and ulcerative colitis also raise your risk
- Fistulas due to obstetric trauma: Obstetric fistulas occur due to prolonged or complicated labor in places with limited access to quality maternal healthcare.
- Risk of fistula formation during healing: Some surgical procedures carry a risk of fistula formation
- Treatment of cancers in the pelvic region can cause the patient to develop a fistula due to radiation damage to tissues.
- Diverticulitis: Inflammation of diverticula (small pouches) in the digestive tract
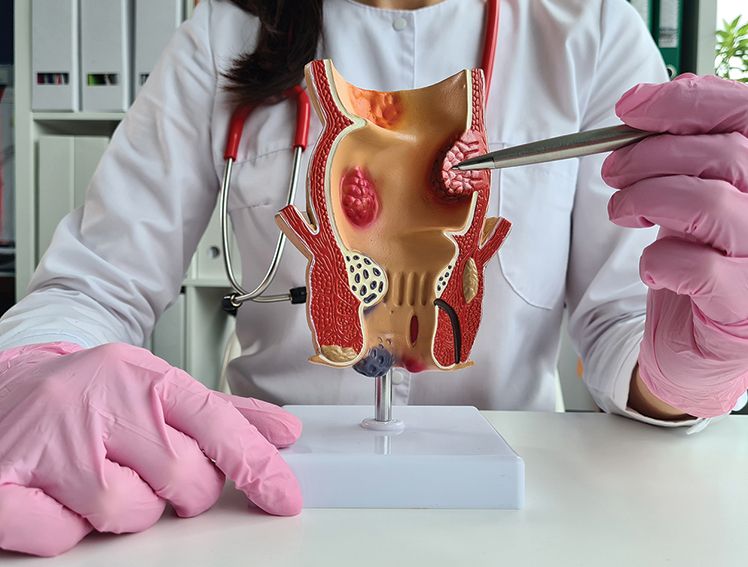
Three Most Common Types of Fistulas
We‘ve already learned that anal fistulas are the most commonly found ones. However, there is a range of other fistulas that you should know about:
- Anal: Fistula growth around the anus can be of three types. When a fistula forms between the anal canal and the skin around the anal opening, it is called anorectal fistula. When a hole develops between the rectum or anus and the vagina, it is called rectovaginal or anovaginal fistula. Sometimes a fistula may occur between the colon and vagina. This is called colovaginal fistula.
- Intestines: When a fistula forms between two parts of an intestine, it is called enteroenteric fistula. Sometimes a fistula may occur between the small intestine and the skin or the colon and the skin.
- Urinary tract: A Fistula between the urinary bladder and the uterus can also occur. Sometimes a hole may develop between the urinary bladder and the vagina, and sometimes between the urethra and the vagina.
Symptoms of fistula – when should you see a doctor
The signs and symptoms of a fistula essentially depend on the part of the body that is affected.
The following are the symptoms of an anal fistula
- Skin irritation and redness around the anus
- Growing pains around the anal region, which gets worse upon sitting, walking or coughing
- Fever associated with chills
- Painful bowel movement and rectal bleeding
- Foul smell from the anus
- Fatigue
- The symptoms of intestinal fitsulas include:
Abdominal pain or pain in the area between the genitals and anus
- Recurrent urinary tract infections
- Severe gas or diarrhea
- Passage of stool or intestinal gas in the stomach, bladder or vagina
- Weight loss
The symptoms of urinary tract fitsulas are:
- Pain while passing urine
- Frequent urination
- Smelly and cloudy urine
- Muddy colored urine
- Passing wind or stools while urinating
What is fistulotomy
Anal fistulas are among the most commonly treated surgical conditions, and fistulotomy is one of the most commonly performed surgical procedures. Fistulotomy differs from complete removal (fistulectomy) of the fistula tract in that it leaves the abnormal pathway open and drains the path as it is opened.
Fistulotomy: An Effective Treatment Approach
When a fistula requires more than just infection control, your doctor may recommend fistulotomy as the most effective treatment option. Fistulotomy is a surgical procedure that involves cutting open the fistula to allow it to heal properly. Depending on the severity of the fistula, your doctor may also use prescription medicines, primarily to manage and control any infections associated with the fistula. However, while medicines help address infections, fistulotomy remains the definitive and most successful method for treating the fistula itself.
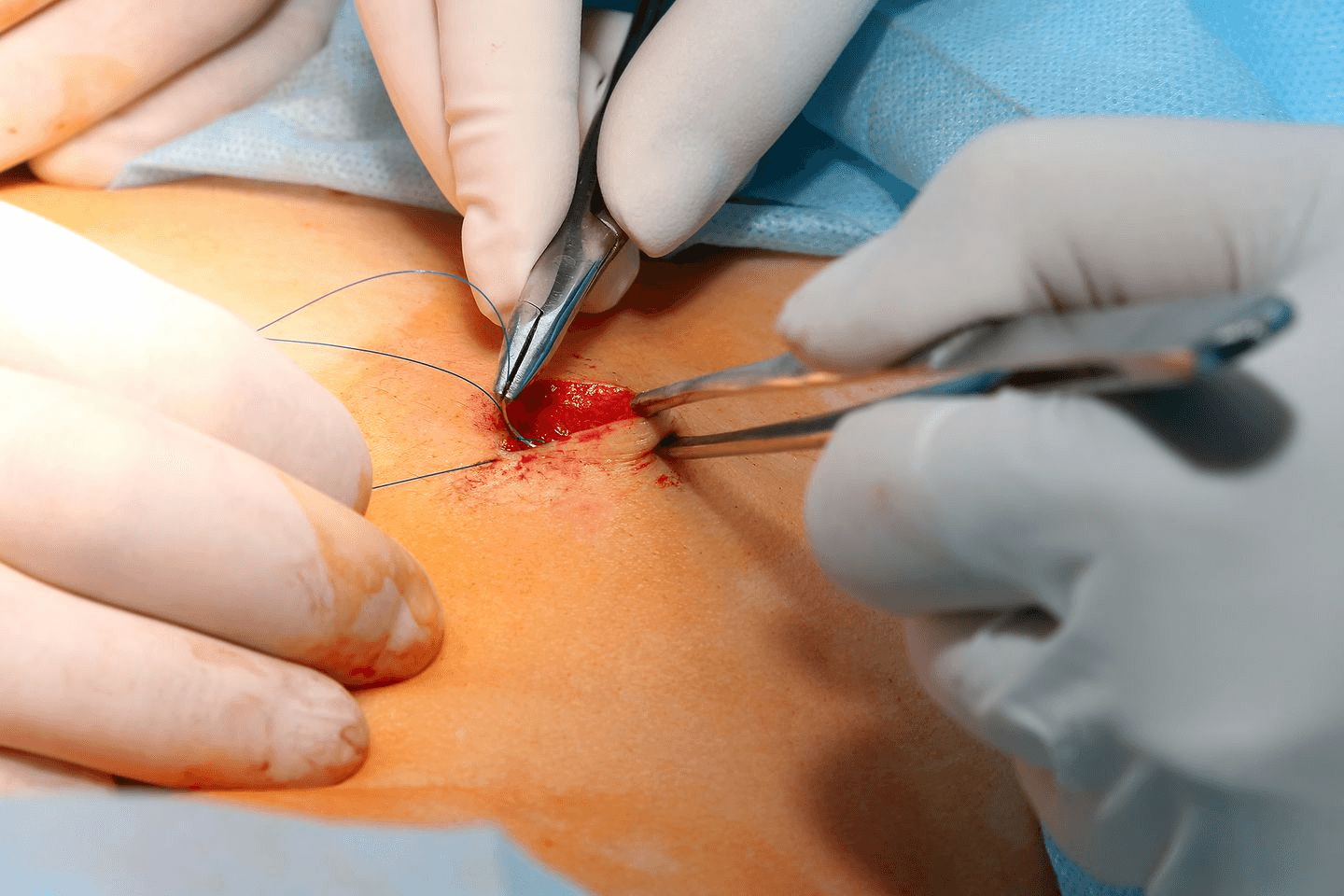
What to expect during fistulotomy
The procedure typically involves:
- Pre-operative assessment: Determining the course and extent of the fistula
- Administration of anaesthesia: Local or regional or, more rarely, general anaesthesia, depending on complexity.
- Surgical opening of the fistula tract to achieve incision and drainage
- Cleaning: Removal of infected tissue and debris from the tract
- Assessment of internal opening: Identification and treatment of the internal opening
- Allowing healing from within: Instead of closing it up, leave it open
Outpatient fistulotomies are most common, and most patients go home the same day. The complexity of the fistula, its location, and the patient's overall good health status will determine how the surgical approach may be modified.
Post-operative Care after Fistulotomy
Proper post-operative care significantly influences recovery outcomes:
- Initial recovery: During the initial recovery, it is normal to experience some discomfort as the effects of the anesthesia gradually fade.
- Wound care: Regular cleaning and dressing changes are essential
- Pain management: Usually managed with over-the-counter or prescription medications
- Sitz baths: Warm water soaks help keep the area clean and promote healing
- Dietary adjustments: Increased fibre and fluid intake help prevent constipation
- Activity restrictions: Temporary limitations on strenuous activities
- Follow-up appointments: Critical for monitoring healing progress
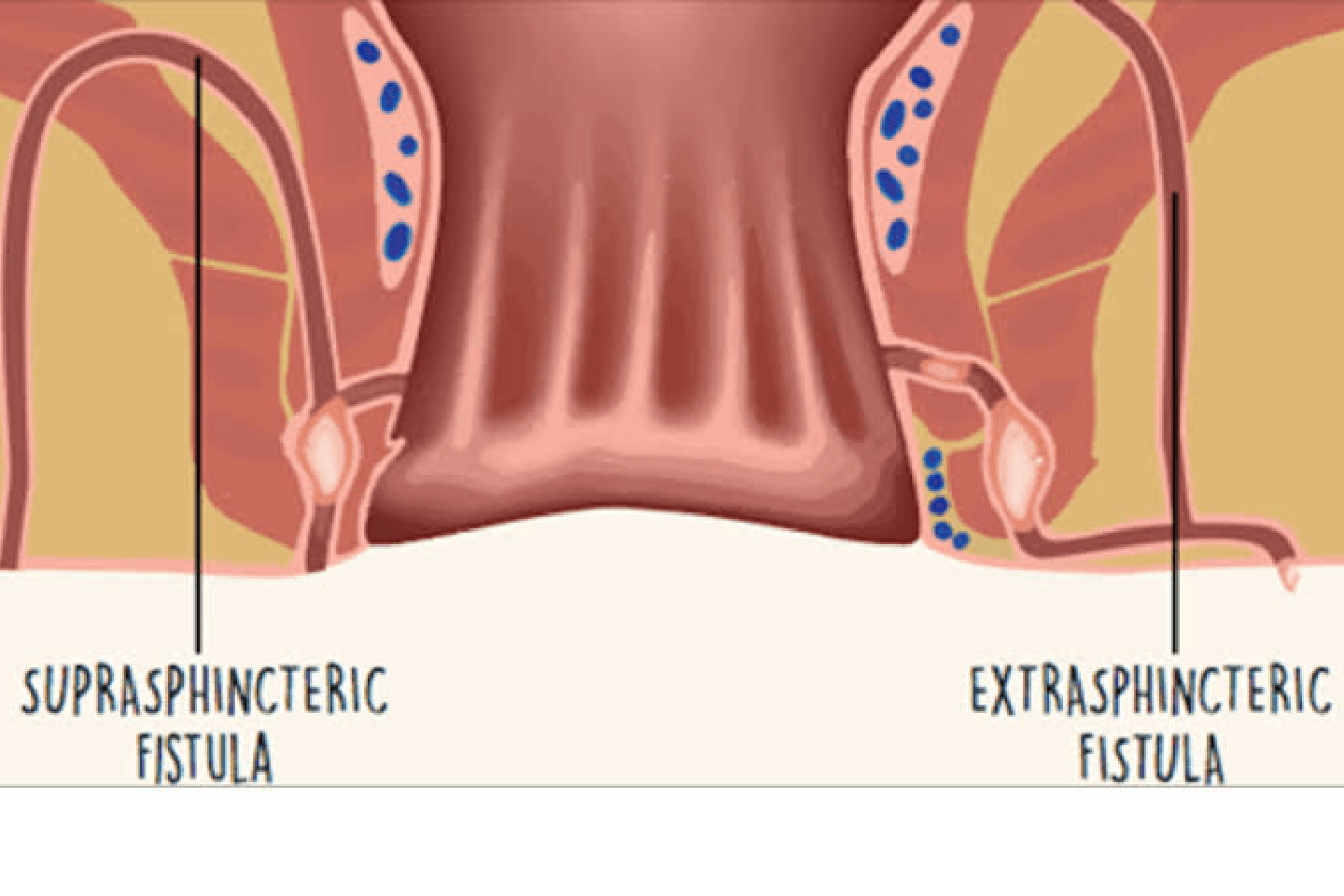
When to Consider Alternative Treatments
While fistulotomy is effective for many cases, alternative approaches may be recommended for:
- Complex or deep fistulas
- Fistulas in patients with inflammatory bowel disease
- Recurrent fistulas
- High anal fistulas where fistulotomy might compromise continence
Conclusion
Fistulas, though uncomfortable and concerning, are treatable medical conditions. Procedures such as fistulotomy can prevent complications and symptoms and be used to resolve them promptly. A healthcare professional should be consulted if you’re experiencing symptoms that suggest a fistula. With modern surgical techniques of fistulotomy, minimally invasive treatments with high success have a relatively quick recovery.